Borderline Personality Disorder (BPD) and Eating Disorders (ED) are two complex conditions that can devastate someone’s life. Understanding the comorbidity between these disorders involves exploring their definitions, the different types of Eating Disorders, the links between BPD and Eating Disorders, their causes, treatment approaches, and a summarizing overview of these interconnections.
BPD is a mental health condition characterized by a pattern of intense instability in moods, behavior, self-image, and functioning. These symptoms frequently result in high levels of impulsivity, and unstable relationships. People with BPD may experience severe episodes of anger, depression, and anxiety. These episode may last a few hours to a few days.
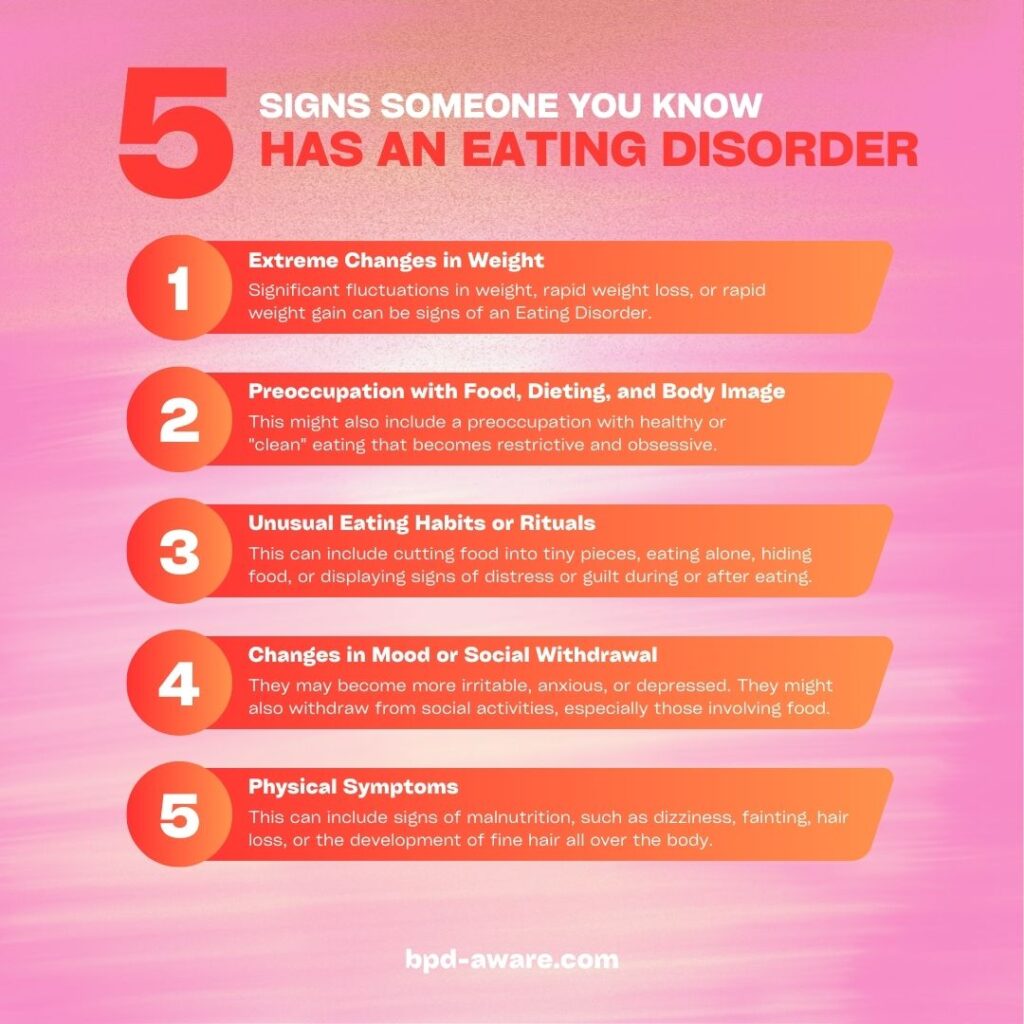
Eating Disorders are conditions in which an unhealthy relationship with food negatively affects a person’s physical and mental health. EDs include extreme emotions, attitudes, and behaviors surrounding weight and food issues.
Types of Eating Disorders
There are a number of Eating Disorders, including (but not limited to):
- Anorexia Nervosa: Characterized by weight loss (often due to severe restriction of food intake), an strong fear of gaining weight, and a distorted body image.
- Bulimia Nervosa: Involves episodes of binging followed by purging to prevent weight gain, which can include vomiting, excessive use of laxatives, or extreme exercise.
- Binge Eating Disorder (BED): Similar to Bulimia Nervosa but without the regular use of purging to avoid weight gain. People with BED engage in episodes of eating large quantities of food but do not regularly use purging behaviors.
- Avoidant/Restrictive Food Intake Disorder (ARFID): Unlike other Eating Disorders, ARFID does not involve distress about body shape or size or a desire to lose weight. Instead, it is characterized by a significant lack of desire in eating food, or avoidance based on the characteristics of food, or a past negative experience with food.
How Eating Disorders Develop
The development of Eating Disorders is a complex process influenced by a combination of genetic, biological, psychological, and sociocultural factors. No single cause has been identified; rather, it’s a combination of these factors that usually leads to the onset of an Eating Disorder. Understanding this multifaceted development process is crucial for recognizing vulnerabilities and implementing effective prevention and treatment strategies.
Here’s a breakdown of the factors involved:
Genetic and Biological Factors
- Genetic Predisposition: Research suggests that Eating Disorders can run in families, indicating a genetic component. Individuals with a close relative (parent or sibling) who has an ED are at a higher risk of developing one themselves.
- Brain Chemistry: Neurotransmitters, the chemicals in the brain that communicate information throughout our brain and body, play a role in eating behaviors. Imbalances in neurotransmitters like serotonin and dopamine might influence Eating Disorder behaviors.
- Brain Structure and Function: Differences in the physical structure and function of precise brain areas that regulate appetite, reward, and self-control might contribute to the susceptibility to Eating Disorders.
Psychological Factors
- Emotional Regulation: Difficulty in managing emotions can lead individuals to turn to disordered eating behaviors as a coping mechanism.
- Perfectionism: A personality characterized by striving for flawlessness and setting high-performance standards can be at risk, particularly when combined with critical self-evaluation.
- Low Self-Esteem: Negative self-perception and dissatisfaction with one’s body can drive disordered eating as a means to achieve an idealized body image.
- Trauma and Stress: Experiencing trauma, such as physical or sexual abuse, as well as chronic stress, can heighten the risk of developing an Eating Disorder.
Socio-cultural Factors
- Media and Cultural Influences: The portrayal of ideal body types in media and cultural norms emphasizing thinness or muscularity can contribute to body dissatisfaction and the pursuit of weight loss or body shaping through unhealthy behaviors.
- Social Pressure and Bullying: Peer pressure regarding appearance and weight, along with bullying or teasing, can lead to a poor body image. The negative body image then leads to Eating Disorders.
- Family Dynamics: Family attitudes and behaviors concerning weight and diet, as well as family conflicts, can influence Eating Disorder development.
The Development Process
The process by which Eating Disorders develop often involves an interaction of these factors, which can trigger or exacerbate one another. For example:
- Initiation: It might start with a simple diet or an attempt to improve fitness, influenced by personal insecurities, societal pressures, or comments from peers or family. For someone with a genetic predisposition and psychological vulnerabilities, what starts as a benign attempt to eat healthier or lose a little weight can spiral into an obsession.
- Progression: As the individual receives positive reinforcement for weight loss or changes in eating habits (either from themselves, peers, or media), the behaviors become more entrenched. Psychological factors, such as a need for control or a way to cope with negative emotions, can make these behaviors more appealing and harder to break.
- Maintenance: Over time, Eating Disorder behaviors can become a primary way of coping with stress, regulating emotions, or maintaining a sense of control in life. This can be reinforced by continued societal pressures and possibly exacerbated by the physical effects of malnutrition on the brain, making it increasingly difficult to return to healthy eating habits without help.
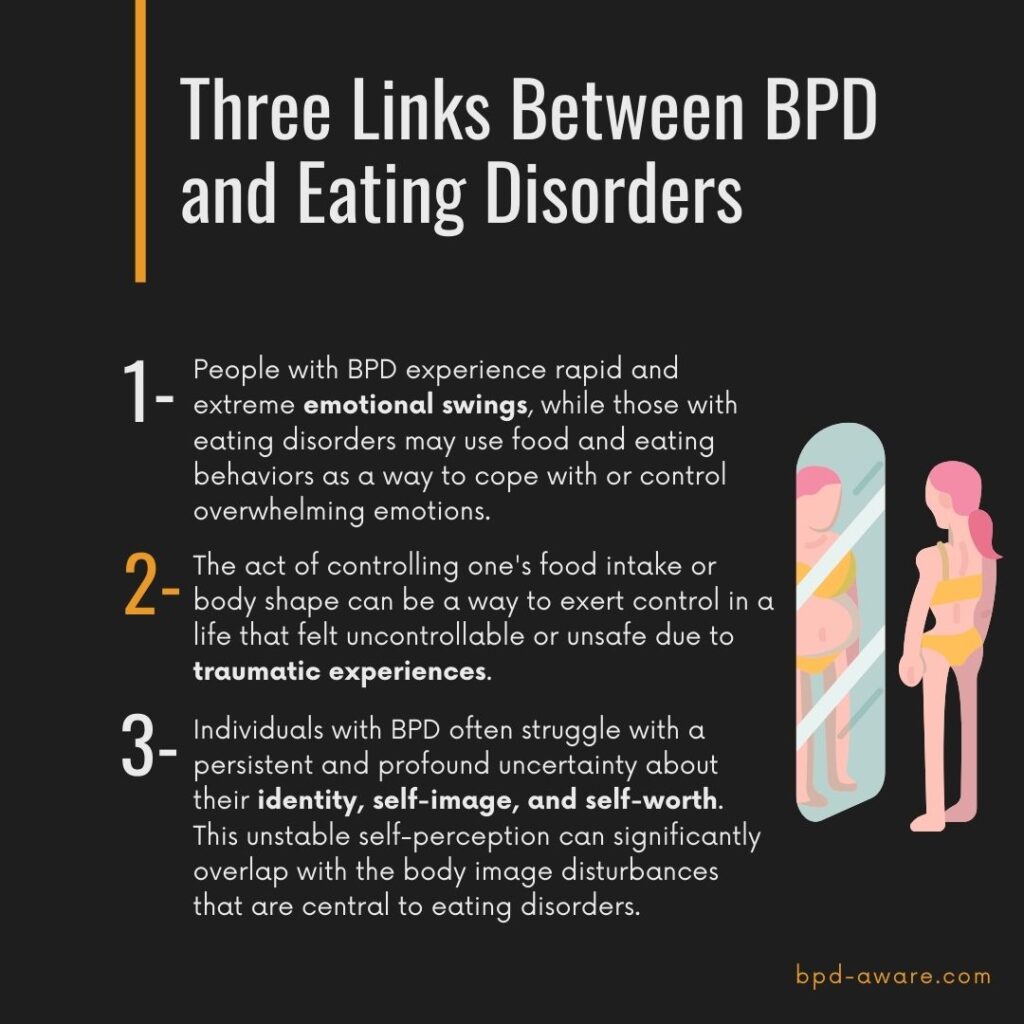
Links Between BPD and Eating Disorders
The links between BPD and Eating Disorders are complex and multifaceted. Research suggests that individuals with BPD are at a higher risk of developing Eating Disorders, and vice versa. One study has reported that over HALF of all people with BPD meet the criteria for also having an Eating Disorder.
This co-occurence can be attributed to several important factors:
- Emotional Dysregulation: Both disorders involve significant difficulties in managing emotions. The impulsivity and emotional instability characteristic of BPD can lead to unhealthy eating behaviors as a coping mechanism.
- Trauma and Stress: Individuals with BPD often have a history of trauma or chronic stress, which are also risk factors for the development of Eating Disorders.
- Identity Issues: People with BPD may struggle with a sense of identity, which can contribute to body image issues. They may attempt to control aspects of their identity through food and develop an Eating Disorder as a result.
Self-Destructive Tendencies
Eating Disorders often serve as a maladaptive method for individuals with Borderline Personality Disorder to express and manage self-destructive tendencies, using their relationship with food as the medium. For instance, the act of binge eating can be seen as an attempt to temporarily quell the pervasive feelings of emptiness that plague those with BPD, effectively “filling” the emotional void with food. Conversely, purging, whether through vomiting or excessive exercise, can induce a fleeting sense of euphoria or relief, offering a short-term escape from the intense and fluctuating emotions of anger common in BPD, only to be followed by exhaustion.
These disorders emerge as flawed coping mechanisms, aiming to shift focus away from the perceived turmoil of their external environment to something they feel they can control: their body and food intake. This can manifest in various forms of disordered eating, such as restricting food intake as seen in Anorexia Nervosa, to gain a sense of control over one’s life, or binge eating followed by purging in Bulimia Nervosa, as a way to both experience and then expel overwhelming emotions. Each of these behaviors, from starvation to overeating and purging, represents an attempt to self-regulate and soothe emotional distress, albeit in a harmful and ultimately unsustainable manner.
For example, someone might turn to excessive eating (Binge-Eating Disorder) or engage in binge-purge cycles (Bulimia Nervosa) to suppress or “stuff down” difficult emotions. Alternatively, an individual might restrict food intake (Anorexia Nervosa) as a means to numb their feelings, creating a sense of detachment from emotional pain.
The trigger for these Eating Disorders is often not physical hunger but rather emotional hunger, where emotional states—be they anxiety, boredom, anger, frustration, or irritability—dictate eating behaviors rather than genuine physiological needs. This can lead to patterns where emotions drive someone to either consume more food than is physically necessary or to limit intake excessively, regardless of the body’s actual hunger signals. For instance, a person feeling anxious or stressed might find themselves eating excessively without physical hunger cues or, conversely, losing their appetite entirely due to emotional turmoil.
Control
Eating Disorders can provide a false sense of control in two main ways:
- Regulating Emotions: For someone with BPD, the act of controlling food intake or engaging in compensatory behaviors like purging can serve as a means to manage or numb overwhelming emotions. For instance, the restrictive behaviors in Anorexia Nervosa may be perceived as a way to maintain discipline or order amidst emotional chaos, while binge eating can temporarily soothe feelings of emptiness or loneliness.
- Shaping Identity: The control over body weight and shape becomes a tangible metric of self-worth and identity for many individuals with BPD and Eating Disorders. Achieving a certain body image or weight can become intertwined with their sense of self and perceived control over their lives.
Examples of Control through Eating Disorders
- In Anorexia Nervosa, the meticulous control over calorie intake and weight can give an individual a sense of mastery over their body, which contrasts sharply with the perceived lack of control over their emotional world. The discipline required to maintain such control can be seen as a personal achievement and a way to define oneself.
- Bulimia Nervosa involves cycles of binging and purging that may provide momentary relief from emotional distress or self-loathing. The purging phase, in particular, can be viewed as an attempt to regain control after the perceived loss of control during binging.
- Individuals with Binge-Eating Disorder might use food to fill an emotional void or cope with feelings of stress and anxiety, temporarily creating a sense of emotional regulation or control, even as it spirals out of control physically.
The Paradox of Control
Ironically, while Eating Disorders may initially offer an illusion of control, they ultimately lead to a greater loss of control—over one’s health, emotions, and life. This paradox underscores the destructive nature of using Eating Disorders as a coping mechanism for BPD.
Treatment Implications
Effective treatment for individuals with BPD and comorbid Eating Disorders often involves addressing the underlying need for control and developing healthier coping mechanisms. Therapies like Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT) can be effective, as they focus on building emotional regulation skills, enhancing self-esteem, and fostering a healthier relationship with food and one’s body.
Treating an individual with Borderline Personality Disorder (BPD) and a comorbid Eating Disorder presents unique challenges due to the complex interplay between the emotional dysregulation, identity issues, and maladaptive coping mechanisms characteristic of BPD and the severe physical and psychological risks associated with Eating Disorders. Effective treatment typically requires a comprehensive, multi-disciplinary approach that addresses both sets of disorders simultaneously. Here are key components and approaches in the treatment of someone with BPD and a comorbid Eating Disorder:
1. Integrated Treatment Plan
An integrated treatment plan that addresses both BPD and Eating Disorders concurrently is crucial, as these conditions often influence and exacerbate each other. This plan should include a combination of psychotherapy, medical management, nutritional counseling, and, when necessary, medication.
2. Therapy
Several therapeutic approaches are effective for treating BPD and comorbid Eating Disorders:
- Dialectical Behavior Therapy (DBT): Originally developed for BPD, DBT is highly effective for patients with comorbid Eating Disorders. DBT teaches skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. DBT helps people understand and accept their feelings, learn better ways to cope with distress, and improve relationships with others.
- Cognitive Behavioral Therapy (CBT): CBT can be adapted to address Eating Disorders by helping individuals identify and challenge distorted thoughts about food, body image, and self-worth, and develop healthier eating behaviors.
- Schema Therapy: This approach is particularly useful for those with BPD, focusing on identifying and changing deeply held patterns of thinking and behavior that underlie the disorder.
3. Medical Management and Nutritional Counseling
Medical oversight is critical, as Eating Disorders can lead to severe physical health complications. Regular monitoring of vital signs, electrolytes, and overall physical health is necessary. Nutritional counseling with a dietitian specialized in Eating Disorders is essential to help the individual develop a healthy relationship with food, understand nutritional needs, and create a balanced meal plan.
4. Medication
While there are no medications specifically designed to treat BPD, certain medications can help manage symptoms of both BPD and Eating Disorders, including:
- Antidepressants: Can help manage symptoms associated with depression and anxiety.
- Mood Stabilizers: Can be used to reduce impulsive behavior and mood swings.
- Antipsychotics: In low doses, can help reduce symptoms of thought distortion, paranoia, and dissociation.
It’s important to note that medication should be used as part of a broader treatment plan and not as a sole treatment option.
5. Hospitalization
In some cases, especially when there’s a risk of suicide or severe self-harm, or if the Eating Disorder has led to critical health issues, hospitalization may be necessary. This can provide a safe environment for stabilization, intensive therapy, and medical treatment.
6. Family Therapy
Including family members in the treatment process can be beneficial, especially for adolescents. Family therapy can help resolve conflicts, make communication more effective, and educate family members about BPD and Eating Disorders, enabling them to support the individual’s recovery.
7. Support Groups
Participation in support groups can offer valuable social support, reduce feelings of isolation, and provide a forum for sharing strategies for coping with both BPD and Eating Disorders.
Final Thoughts
The treatment of BPD and a comorbid Eating Disorder requires a tailored, interdisciplinary approach that addresses the multifaceted nature of these conditions. Success often depends on a combination of psychotherapy, proper medical care, support, and, importantly, the individual’s commitment to recovery. Given the complexity of these disorders, treatment is usually long-term, focusing on managing symptoms, improving quality of life, and supporting the individual in achieving a healthier relationship with themselves and their eating behaviors.
Sources, Resources, and Further Reading
- Dysregulated Eating Behaviors in Borderline Personality Disorder: Are Rejection Sensitivity and Emotion Dysregulation Linking Mechanisms?: https://pmc.ncbi.nlm.nih.gov/articles/PMC4243037/
- Eating disorders among patients with borderline personality disorder: https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-020-00314-3
- I Hate You, Don’t Leave Me; I’m Hungry, Don’t Feed Me: https://www.psychologytoday.com/us/blog/i-hate-you-dont-leave-me/201909/i-hate-you-dont-leave-me-im-hungry-dont-feed-me
- Surprising Link Between Eating Disorders and BPD Nobody Tells You: https://www.youtube.com/watch?v=g-0CRfg3RLQ
- Treat Co-Occurring Eating Disorders and Borderline Personality Disorder: https://www.eatingdisorderhope.com/treatment-for-eating-disorders/co-occurring-dual-diagnosis/borderline-personality-disorder