Dialectical Behavior Therapy (DBT) is a type of talk therapy (aka psychotherapy) designed for people who experience a very intense range of emotions. It was created by Dr Marsha Linehan when she was treating people she would later recognize to have Borderline Personality Disorder (BPD).
Traditional talk therapy requires a patient to come in and be willing to discuss their problems while the therapist listens and asks questions. The information from these sessions would allow the therapist to root out problems and provide ideas for improving the situation. However, due to the sensitive nature of people with BPD, this often caused a backlash from the patient, who saw the advice as being told they were the problem. A more accepting form of therapy where a therapist would validate the patient’s experiences without offering advice wouldn’t work either, as the patient felt they weren’t receiving any help.
Instead, DBT combines these two approaches, offering the patient both validation and methods of change.
What is Dialectical Behavior Therapy Used For?
As well as treating Borderline Personality Disorder of all four subtypes (discouraged, impulsive, petulant, and self-destructive), DBT can be used to treat a wide range of mental health conditions such as:
- Bipolar disorder.
- Depression.
- Anxiety.
- Suicidal behavior.
- Self-harm.
- Substance abuse.
- Eating disorders.
What is Dialectical Behavior Therapy?
Dialectical Behavior Therapy consists of four core components:
- A skills training group.
- Individual talk therapy.
- Telephone consultation.
- A therapist consultation team.
The skills training group is designed to help patients target negative behavioral responses that cause instability and duress and replace them with positive responses. The group will typically meet once a week for two hours, and the course will take around six months to complete.
Patients can repeat the course or specific modules if they feel it is beneficial. During the course, they will be given homework to reinforce what they have learned and to help turn the new skills into consistent, positive habits.
Skills Training Group
The skills training group focuses on mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance.
The mindfulness portion of the course teaches patients how to be present in the moment – processing what they are thinking and feeling and calmly accepting these sensations. The mindfulness skills are separated into “what” and “how” skills. The patient is taught how to observe, describe, and participate fully in the moment during the “what” skills portion. What is happening around you? What emotions are you feeling? What do these emotions make you want to do? This level of mindfulness will help to reduce impulsive or emotionally charged behavior.
The “how” skills help teach patients not to judge themselves negatively for their emotional responses. This helps the patient avoid triggering negative behavioral responses.
The interpersonal skills section of the course focuses on how to socialize with others effectively. People with borderline personality disorder have often suffered a form (or multiple forms) of abuse during their upbringing that has left them with poor social skills that have been built up as a defense mechanism. These poor social skills tend to lead to tumultuous relationships, which leads to more poor social skills and defense mechanisms. The patient will be taught how to recognize what they need from a relationship, how to ask for it appropriately, how to say “no” to inappropriate demands from others, and how to cope with conflict.
People with BPD often suffer from intense and volatile emotions. The emotion regulation module of DBT begins with identifying emotions and emotional responses so the patient can recognize how one leads to the other. Patients will learn how to identify roadblocks to changing their emotions and how best to deal with them. Patients are taught how to avoid negative situations that lead to negative emotions and how to increase positive situations in their lives instead.
By trying to avoid distress altogether, as some people with BPD do, you are missing out on many aspects of life, as well as further weakening your tolerance of distress when it inevitably occurs. The Distress tolerance module will teach patients that emotional pain and times of suffering are inevitable and should be accepted as part of life. Patients will be taught how to survive crises by adjusting their thoughts, distracting themselves, and self-soothing. Acceptance skills will also be taught to help patients, making previously intolerable emotional pain much more bearable.
Individual Talk Therapy
Individual talk therapy is what many would consider the standard therapy experience. The patient and therapist will meet regularly to discuss what’s going on in the client’s life with a focus on how it relates to their BPD and the treatment they’re receiving. There are six main areas of focus: parasuicidal behaviors, therapy-interfering behaviors, behaviors that interfere with quality of life, behavioral skills acquisition, post-traumatic stress behaviors, and self-respect behaviors.
If a patient is feeling suicidal, this needs to be discussed and explored in detail. The therapist will teach the patient coping and distress management techniques to help ease the burden of these thoughts and feelings. Problem-solving behaviors will also be taught to stop recurring triggers that lead to suicidal thoughts.
The patient and the therapist can both cause therapy-interfering behaviors and need to be discussed openly and with as little judgment as possible. While the client more often demonstrates therapy-interfering behaviors, the therapist can cause issues themselves if, for example, they’re not perceived to be actively listening to the client.
Other examples of therapy-interfering behaviors include poor attendance/repeat tardiness, argumentative behavior, and noncompliance.
Behaviors that disrupt quality of life include substance abuse, risky sexual behavior, gambling, financial insecurity, and anything else that may harm the client’s physical or mental health.
Acquiring positive behavioral skills is vital in helping the client improve their life. These skills are taught in the skills training group, and progress and improvement ideas will be discussed during the individual talk therapy.
Many people with Borderline Personality Disorder have suffered through one or more traumatic events during their lives. Discussing these events only when the patient feels emotionally ready is essential. This can be one of the most challenging elements of talk therapy as it involves dredging up memories that many clients would rather forget. However, therapy can help re-frame these events and help the client reduce any blame they put on themselves and reduce intrusive thoughts caused by the event.
Lastly, the therapist will reinforce behaviors that show clients respect for themselves. This includes saying no to others, talking about yourself positively and realistically, and surrounding yourself with people who treat you well.
Telephone Consultation
Telephone consultations allow patients quick (although not necessarily immediate) access to their therapist for in-the-moment guidance and emergencies. These phone calls are designed and structured to help teach the patient how and when to ask for help, asking for help in the earliest stage of a crisis before it snowballs into something bigger. This allows the therapist to assist before the patient has engaged in a negative behavior such as self-harm.
These phone calls typically occur as and when needed, although the therapist may limit them to specific times for the sake of the client’s mental health.
Therapist Consultation Team
The DBT consultation team typically includes three to eight therapists, who meet regularly—often weekly—to discuss their patients’ progress and their responses to sessions. Therapists can also discuss potential strategies for best helping a patient from their current state. These sessions are also a form of self-therapy for the therapy team. Treating individuals with BPD can be incredibly stressful, and the team consultation allows the therapists to help one another manage the stress and strain this can put on their own lives.
Patients do not attend these meetings.
How Effective is Dialectical Behavioral Therapy in Treating Borderline Personality Disorder?
77% of people who underwent DBT to treat BPD no longer met the criteria for borderline personality disorder after the conclusion of treatment. This impressive recovery rate is why Dialectical Behavioral Therapy is considered the best option for treating Borderline Personality Disorder. However, that does mean that DBT isn’t effective for everyone. There are other therapeutic options used to treat BPD, such as Schema Therapy and Mentalization-Based Therapy, which can be used when DBT proves to be ineffective.
Treatment typically takes at least six months to a year. Depending on various factors, though, it can take several years. It’s important to remember that “getting better” at anything is seldom a straight upward line—there are always peaks and troughs—and therapy is no different.
Questions to Ask a Therapist Before Visiting Them
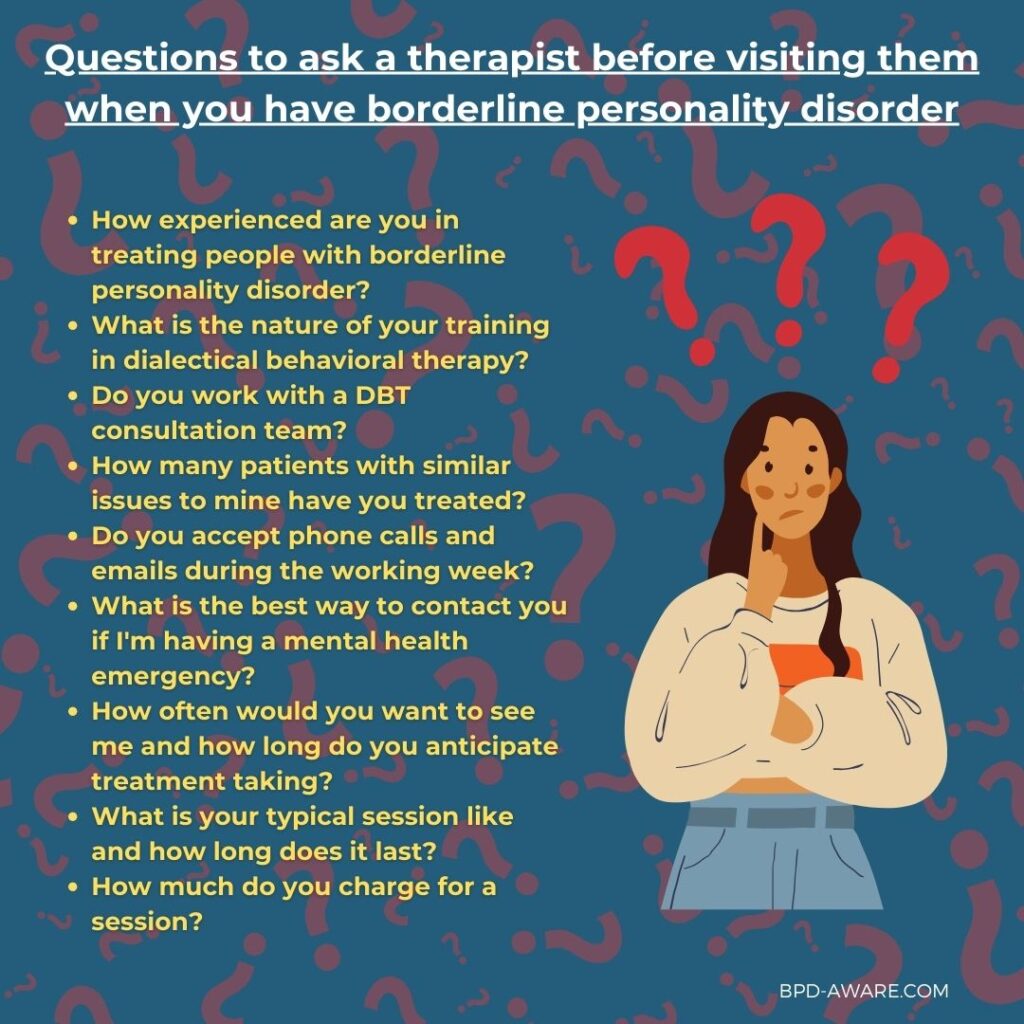
Before you visit a therapist to seek treatment for Borderline Personality Disorder, it’s essential to make sure they are the right therapists to help you improve your mental health. Choosing the wrong therapist can cost you time, money, and your mental health, so it’s important to ask questions and get a feel for them before you make an appointment.
Important questions include:
- How experienced are you in treating people with Borderline Personality Disorder?
- What is the nature of your training in Dialectical Behavior Therapy?
- Do you work with a DBT consultation team?
- How many patients with similar issues to mine have you treated?
- Do you accept phone calls and emails during the working week?
- What is the best way to contact you if I’m having a mental health emergency?
- How often would you want to see me, and how long do you anticipate treatment taking?
- What is your typical session like, and how long does it last?
- How much do you charge for a session?
Sources, Resources, and Further Reading
- How Dialectical Behavior Therapy Can Help People with BPD: https://psychcentral.com/disorders/borderline-personality-disorder/borderline-personality-disorder-dialectical-behavior-therapy
- DBT for Borderline Personality Disorder (BPD): What to Expect & How It Works: https://www.choosingtherapy.com/dbt-for-bpd/
- Comparison of 8-vs-12 weeks, adapted dialectical behavioral therapy (DBT) for borderline personality disorder in routine psychiatric inpatient treatment—A naturalistic study: https://www.nature.com/articles/s41598-024-61795-9
- Dialectical behaviour therapy for women with borderline personality disorder: https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/dialectical-behaviour-therapy-for-women-with-borderline-personality-disorder/B18DBB959BC4613E920EA330E1625E5F
- Dialectical Behavior Therapy for Borderline Personality Disorder: An Overview: https://alterbehavioralhealth.com/blog/dbt-for-borderline-personality-disorder/