While the precise causes of Borderline Personality Disorder (BPD) are multifaceted, involving genetic, environmental, and social factors, a growing body of research highlights a significant link between childhood trauma and the development of BPD. This article delves into how childhood trauma can lead to BPD, the changes in brain chemistry associated with it, the different types of childhood trauma, and the approaches to treating both trauma and BPD.
The Connection Between Childhood Trauma and BPD
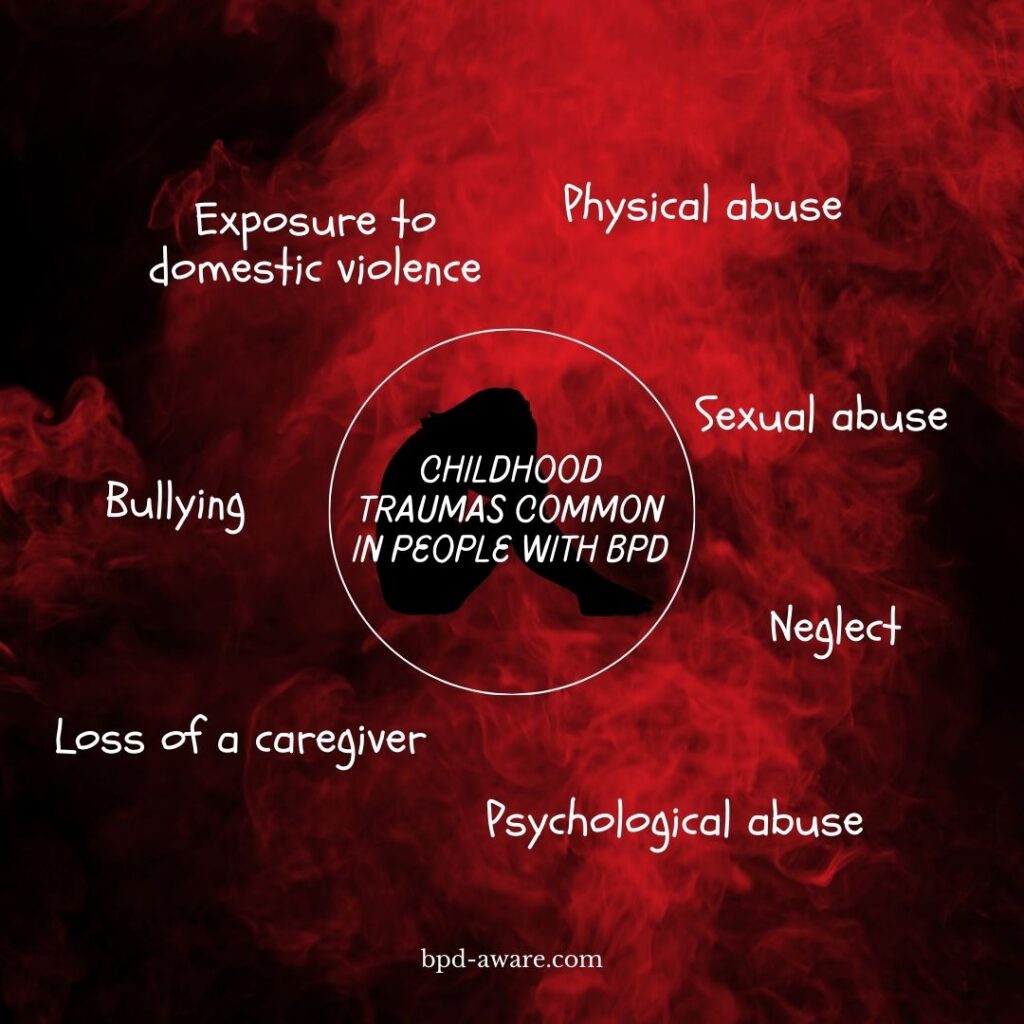
Childhood trauma, defined as a deeply distressing or disturbing experience during one’s childhood, can take various forms. These forms can include physical, sexual, and emotional abuse, loss of a caregiver, neglect, and exposure to domestic violence or substance abuse. These traumatic experiences can profoundly impact a child’s developing brain, influencing the development of BPD in several ways.
Emotional Dysregulation and Hyperarousal
Childhood trauma can lead to persistent states of hyperarousal, where the individual is constantly on alert for threats. This heightened state of arousal makes it challenging for the brain to process emotions in a balanced manner, leading to the emotional volatility seen in BPD. The brain’s development is altered in such a way that the regulation of emotions becomes skewed, with trauma survivors often experiencing emotions more intensely and for longer durations than those without such histories. The dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress response, further exacerbates this emotional sensitivity, making individuals more reactive to stress and perceived threats of abandonment or rejection.
Disrupted Attachment and Interpersonal Relationships
The quality of early relationships, particularly with caregivers, plays a pivotal role in the development of BPD. Traumatic experiences, such as abuse, neglect, or early parental loss, can severely disrupt the formation of secure attachments. This disruption can lead to an intense fear of abandonment, a core feature of BPD. People can develop maladaptive coping mechanisms, such as clinging to relationships or rapidly cycling between idealization and devaluation of others, in an attempt to manage these fears. These patterns are often rooted in the instability and unpredictability of their early life experiences, reflecting an internal struggle to find safety and stability in relationships.
Impaired Self-Identity
Childhood trauma can also profoundly affect the development of a coherent sense of self. Traumatized individuals may struggle with feelings of emptiness, identity confusion, and a chronic sense of worthlessness, symptoms that are prominently featured in BPD. The inconsistency and unpredictability of a traumatic childhood environment can prevent the development of a stable self-image. As a result, individuals with BPD often experience significant difficulties in knowing who they are and what they value, leading to a persistent sense of emptiness and a lack of a consistent sense of identity.
Biological Underpinnings
The link between childhood trauma and BPD is also supported by biological evidence. Neuroimaging studies have shown that individuals with BPD, particularly those with histories of trauma, exhibit structural and functional abnormalities in regions of the brain involved in emotion regulation, impulse control, and stress response, such as the amygdala, hippocampus, and prefrontal cortex. These changes can contribute to the symptomatology of BPD, including emotional instability, impulsivity, and difficulties in managing stress and fear responses.
Types of Childhood Trauma
Understanding the different types of childhood trauma can help in identifying the roots of BPD and tailoring treatment approaches. The main types include:
Physical Abuse
Physical abuse involves inflicting physical harm upon a child through actions such as hitting, beating, burning, or physically harming them in any way. This form of trauma is characterized by bodily injuries but can also lead to severe emotional and psychological scars. Children who experience physical abuse may develop a variety of emotional problems, including anxiety, depression, and issues related to self-esteem and trust.
Sexual Abuse
Any sexual activity with a child is considered abuse, whether by an adult, an older or more powerful child, or even someone of the same age if there is a significant imbalance of power or understanding. This can involve direct physical sexual acts, exposure, voyeurism, and involvement in pornography. The impact of sexual abuse is profound, often resulting in long-term emotional and psychological difficulties, such as PTSD, sexual dysfunction, and relationship problems.
Emotional or Psychological Abuse
Emotional or psychological abuse involves actions and behaviors that harm a child’s self-esteem and emotional well-being. This can include verbal abuse as well as non-verbal actions like neglect, manipulation, or exposure to family violence. Emotional abuse can be just as traumatic as physical abuse, leading to anxiety, depression, and a range of emotional and behavioral issues.
Neglect
Neglect happens when a caregiver doesn’t meet a child’s basic needs, including physical (such as food, clothing, and shelter), emotional (such as affection, attention, and emotional support), medical, and educational needs. Neglect can lead to serious health problems, developmental delays, and emotional issues. Children who experience neglect may struggle with feelings of abandonment, low self-worth, and difficulties in forming healthy relationships.
Exposure to Domestic Violence
Children who witness domestic violence, including physical, sexual, or emotional abuse within their household, experience trauma even if they are not directly abused. Observing violence can lead to feelings of fear, insecurity, confusion, and helplessness. The long-term effects can include emotional distress, difficulty in learning and concentration, a heightened risk of substance abuse, and engaging in volatile relationships in the future.
Bullying
Bullying involves repeated aggressive behavior with the intent to hurt another individual physically, emotionally, or psychologically. It can occur in person or through digital means (cyberbullying). Victims of bullying may experience a range of effects, including social isolation, fear, anxiety, depression, and decreased academic performance.
Traumatic Grief or Separation
Children can experience traumatic grief following the death or loss of a loved one, particularly if the loss is sudden, violent, or involves a perceived or real responsibility on the part of the child. Similarly, traumatic separation from a caregiver, through divorce, incarceration, or removal to foster care, can have lasting impacts. These experiences can lead to profound feelings of grief, anxiety, and insecurity about the world and the stability of their relationships.
Community and School Violence
Exposure to violence. such as witnessing or being a victim of violence, shootings, or other traumatic events, can lead to trauma. This form of trauma can result in a sense of fear and insecurity, affecting a child’s ability to feel safe in their environment.
Natural Disasters and Accidents
Experiencing natural disasters (like earthquakes, floods, and hurricanes) or severe accidents can lead to trauma, characterized by fear, loss, and sometimes displacement. These events can disrupt a child’s sense of safety and normalcy, leading to stress and anxiety disorders.
Systemic and Socioeconomic Trauma
This includes trauma that arises from living in a highly stressful environment due to factors like poverty, discrimination, migration, or being part of a conflict or war-torn community. Such experiences can cause feelings of insecurity, hopelessness, and chronic stress.
Treating Trauma and BPD
Treating individuals with BPD who have experienced childhood trauma requires a multifaceted approach, focusing on both the symptoms of BPD and the underlying trauma.
Psychotherapy remains the cornerstone of treating childhood trauma in adults, with various modalities shown to be effective:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and challenge negative thought patterns and behaviors resulting from past trauma. It’s effective in treating anxiety, depression, and PTSD symptoms related to childhood trauma.
- Dialectical Behavior Therapy (DBT): Originally developed for people with BPD, DBT is effective for individuals with emotional dysregulation and self-harm behaviors stemming from childhood trauma. It emphasizes skills in mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR facilitates the processing of traumatic memories through directed eye movements or other forms of bilateral stimulation. It’s particularly effective for PTSD and can help adults process and integrate traumatic childhood experiences.
- Psychodynamic Therapy: Psychodynamic Therapy focuses on understanding the impact of childhood experiences on current behavior and emotions. It helps individuals explore unresolved issues and the unconscious content of their thoughts and feelings related to trauma.
Trauma-Informed Care
A trauma-informed approach understands the widespread impact of trauma and the potential paths for recovery. It seeks to avoid re-traumatization and is based on principles of safety, trustworthiness, choice, collaboration, and empowerment. Practitioners across all types of services can provide trauma-informed care by being aware of trauma’s effects and integrating this understanding into their practice.
Medication
While no medication can “cure” trauma, certain medications can alleviate symptoms associated with trauma. Antidepressants, anti-anxiety medications, and mood stabilizers may be prescribed as part of a comprehensive treatment plan. Medication can be particularly useful when symptoms are severe enough to interfere with therapy and daily functioning. For more read our article on BPD and medication.
Mindfulness and Body-Centered Therapies
Techniques such as mindfulness, meditation, and yoga can help individuals reconnect with themselves and manage the physiological symptoms of trauma. These practices focus on the present moment and bodily sensations, which can be especially helpful for those who have dissociated from their bodies as a coping mechanism for trauma.
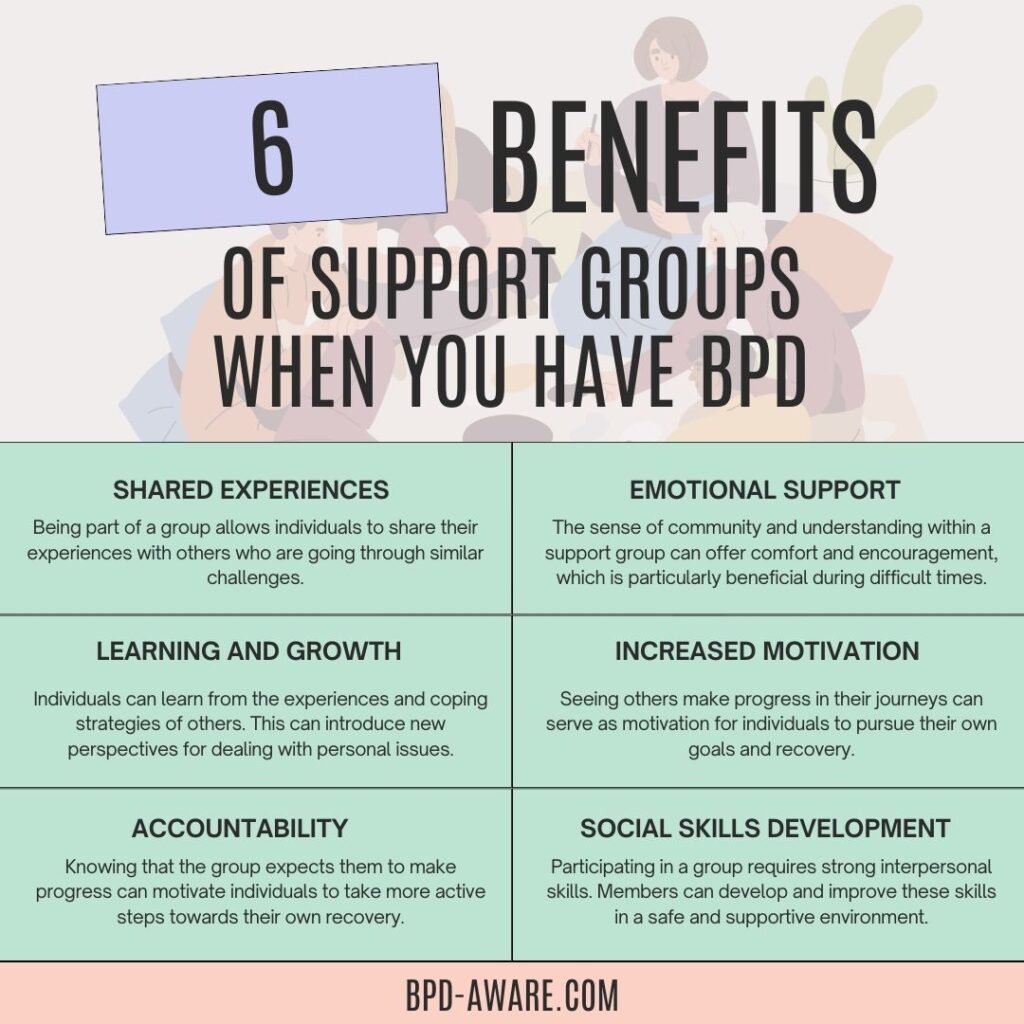
Support Groups
Support groups offer a space for individuals with similar experiences of trauma to share their stories, challenges, and successes. These groups can provide validation, reduce feelings of isolation, and offer peer support and coping strategies.
Creative Therapies
Art therapy, music therapy, and writing can be powerful tools for expressing and processing emotions associated with childhood trauma. These non-verbal therapies can be particularly helpful for individuals who find it difficult to articulate their experiences and feelings.
Lifestyle Changes
Incorporating healthy lifestyle changes can support the recovery process. Regular physical activity, a nutritious diet, sufficient sleep, and avoiding dangerous substances can improve overall well-being and resilience.
Building a Supportive Network
Establishing a network of friends, family, or community members can reduce isolation and provide a great deal of emotional support. Healthy relationships can offer stability, love, and validation that were missing during childhood.
Recognizing the link between childhood trauma and BPD is crucial for developing effective treatment strategies. By addressing both the symptoms of BPD and the underlying trauma, individuals can embark on a path toward healing and improved emotional well-being.
Final Thoughts
Acknowledging the connection between childhood trauma and BPD is crucial for effective treatment. It emphasizes the importance of trauma-informed care in the therapeutic approach to BPD, highlighting the need for interventions that address both the symptoms of the disorder and the trauma underpinnings. This integrated approach can help individuals rebuild a sense of safety and trust, develop healthier relationships, and foster a more stable and coherent sense of self, paving the way for long-term recovery and well-being.
In conclusion, the intricate web linking childhood trauma to the development of BPD underscores the complexity of this condition. Understanding this connection is vital for developing compassionate, effective treatment strategies that address the root causes of the disorder, offering hope and healing to those affected.
Sources, Resources, and Further Reading
- Exploring the Link Between Family Trauma and BPD: https://thewaveclinic.com/blog/exploring-link-between-family-trauma-and-bpd/
- The Role of Trauma in Early Onset Borderline Personality Disorder: A Biopsychosocial Perspective: https://pmc.ncbi.nlm.nih.gov/articles/PMC8495240/
- How Childhood Trauma Can Lead to Borderline Personality Disorder: https://www.psychologytoday.com/us/blog/social-instincts/202108/how-childhood-trauma-can-lead-to-borderline-personality-disorder
- Borderline Personality Disorder has strongest link to childhood trauma: https://www.manchester.ac.uk/about/news/borderline-personality-disorder-has-strongest-link-to-childhood-trauma/