In recent years, the role of diet, particularly sugar consumption, in mental health has gained increasing attention. While the sweet taste of sugar can offer a temporary pleasure or energy boost, its impact on mood, especially among those of us with Borderline Personality Disorder (BPD), can be profoundly negative. This article delves into the mechanisms by which sugar affects mood swings in BPD, offering detailed insights and examples to underscore the importance of dietary mindfulness in managing this condition.
Sugar’s Impact on the Brain
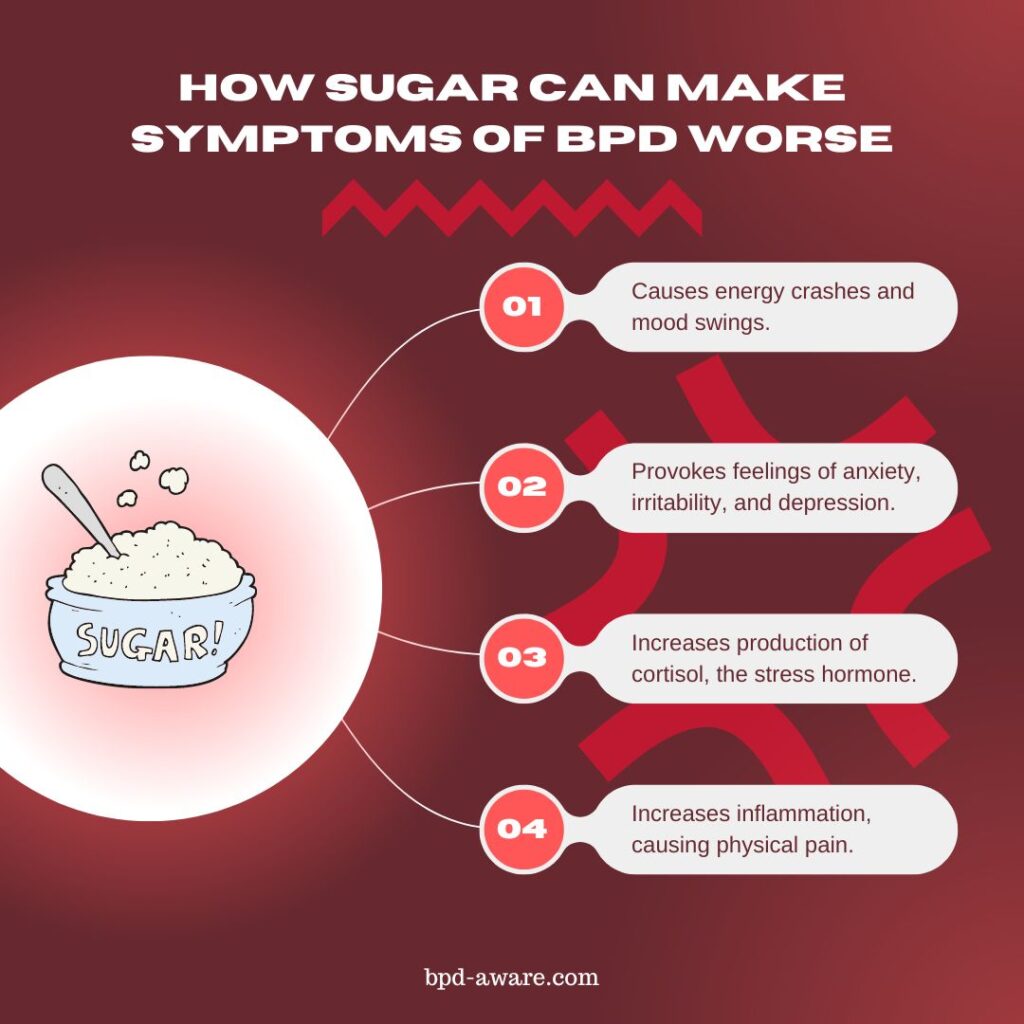
Sugar, particularly in the form of refined sugars found in processed foods, can have an immediate uplifting effect on one’s mood due to the surge in blood glucose levels. This surge leads to a temporary increase in energy and, sometimes, a sense of euphoria. However, this peak is short-lived and is often proceeded by a big dip in blood sugar levels, leading to energy crashes and mood swings. For people with BPD, who already experience intense emotional fluctuations, this cycle can exacerbate their symptoms.
When someone with BPD consumes sugar, the initial spike in blood glucose levels triggers the brain to release “happy” neurotransmitters. However, this is quickly followed by a release of insulin to absorb the excess glucose, leading to a sudden drop in blood sugar levels, often termed a “sugar crash.” This crash can provoke feelings of anxiety, irritability, and depression, intensifying the emotional instability characteristic of BPD.
The (Not So) Sweet Path to Mood Swings
Research has shown that high-sugar diets are associated with an increased risk of various mental health disorders, including depression and anxiety, both of which are common in individuals with BPD. For instance, a study published in the Journal of Psychiatric Research found that participants with high sugar intakes were more likely to experience mood swings, depression, and anxiety.
High sugar intake can stimulate the hypothalamic-pituitary-adrenal (HPA) axis, the body’s main stress response system, leading to increased production of cortisol, the neurotransmitter associated with stress. Elevated cortisol levels can exacerbate mood swings and anxiety.
Consuming too much sugar can lead to a diet lacking essential nutrients, which are crucial for maintaining a stable mood and overall health. Deficiencies in nutrients like magnesium, zinc, and omega-3 fatty acids, all of which play a role in mood regulation, can be particularly detrimental.
The Inflammatory Response
Beyond the immediate impact on blood sugar levels, sugar consumption can also promote inflammation throughout the body, including the brain. Chronic inflammation has been linked to an heightened risk of depression and other psychiatric conditions. For those with BPD, the inflammatory effects of sugar can further destabilize mood, contributing to the severity and frequency of their emotional episodes.
Your blood glucose levels rise every time you consume sugar. To manage this, your body releases insulin. Insulin is a hormone that helps cells absorb glucose for energy or storage. Frequent sugar spikes lead to high levels of insulin in the blood, which can cause systemic inflammation. Over time, this can also lead to insulin resistance, where cells become less responsive to insulin, exacerbating inflammation and increasing the risk of type 2 diabetes.
A diet high in sugar can activate the immune system, leading to the production of pro-inflammatory cytokines. These signaling molecules are part of the body’s natural defense mechanism but, when produced in excess, can cause chronic inflammation.
Too much sugar in your diet can also cause oxidative stress, a condition characterized by an imbalance between free radicals (molecules that damage cells) and antioxidants in your body. This imbalance leads to the damage of proteins, lipids, and DNA, triggering an inflammatory response as the body attempts to repair the damage.
A high-sugar diet can also negatively impact gut health by changing the balance of bacteria in the microbiome. Sugar feeds harmful bacteria and yeast, such as Candida, allowing them to overgrow and disrupt the gut barrier function. This disruption can cause intestinal permeability (often referred to as “leaky gut”), where bacteria and toxins can “leak” into the bloodstream, prompting an inflammatory response from the immune system.
Sugar reacts with proteins and fats in a process known as glycation, forming harmful compounds known as advanced glycation end products (AGEs). AGEs can trigger inflammation by binding to their receptor sites on cells (RAGE), especially in tissues like blood vessels and the skin, contributing to aging and chronic diseases.
The combination of these factors makes it clear why reducing sugar intake is often recommended as a strategy to lower inflammation and improve overall health. By limiting sugar and focusing on a diet rich in whole foods, individuals can mitigate the inflammatory response and protect against the associated health risks, including many of the symptoms of BPD.
How to Reduce Your Sugar Intake
By now you might be getting the idea that consuming sugar is generally a bad idea – and you’re right!
But sugar is addictive and not so easy to quit. It’s in so many foods and drinks that it can be difficult to avoid. However, with some mindfulness, discipline, and forward-planning, it is possible.
The following tips will help you to greatly reduce your sugar intake:
- Understand Your Sugar Intake
Read Labels: Start by reading food labels carefully to identify hidden sugars. Sugar can appear under many names, such as sucrose, high-fructose corn syrup, barley malt, dextrose, maltose, and rice syrup.
Identify Sources: Recognize the primary sources of added sugars in your diet. Common culprits include sodas, candies, baked goods, and even seemingly healthy choices like flavored yogurts and granola bars. - Start Gradually
Reduce Slowly: Abruptly eliminating all sugar from your diet can lead to withdrawal symptoms, including headaches, irritability, and cravings. Gradually reduce your intake to help your body adjust.
Modify Recipes: Lower the amount of sugar in recipes and use natural sweeteners like cinnamon or vanilla extract to add flavor without the extra sugar. - Choose Whole Foods
Focus on Nutrients: Incorporate more whole foods into your diet, such as fruits, vegetables, lean proteins, and whole grains. These foods are naturally lower in sugar and provide essential nutrients that can help balance your diet.
Snack Wisely: Opt for healthy snacks like nuts, seeds, avocado, or whole fruit instead of processed snacks. - Understand and Manage Cravings
Stay Hydrated: What feels like a sugar craving can sometimes be dehydration. Drinking water or herbal teas can help mitigate cravings.
Find Alternatives: When you crave something sweet, have a piece of fruit or a small serving of dark chocolate (with a high percentage of cocoa) to satisfy the craving without consuming too much added sugar. - Be Mindful of Artificial Sweeteners
Use Sparingly: While they don’t raise blood sugar levels, artificial sweeteners can still maintain the taste for sweetness, potentially keeping cravings alive. Some research also suggests they may have undesirable effects on gut health and metabolism. - Prepare for Social Situations
Plan Ahead: Social gatherings often present a challenge with an abundance of sugary options. Eat a healthy meal before attending, or bring a dish that fits your dietary goals. - Educate Yourself
Learn About Sugar: Understanding the impact of sugar on your health can be a powerful motivator. Educating yourself about how sugar affects your body and mind can strengthen your resolve to cut it out. - Seek Support
Community Help: Joining a support group or community of individuals with similar goals can provide encouragement and accountability. Friends and family can also offer support. - Monitor Your Progress
Keep a Food Diary: Tracking what you eat can help you become more aware of your sugar intake and motivate you to keep reducing it. - Adjust Your Environment
Clear Out Temptations: Remove sugary snacks from your home and replace them with healthier options. Making sugar less accessible helps reduce consumption.
Final Thoughts
While sugar might offer a fleeting sense of pleasure, its impact on individuals with BPD can be profoundly negative, exacerbating mood swings and emotional instability. By understanding the biochemical and psychological effects of sugar, those affected by BPD can take proactive steps towards stabilizing their mood through mindful dietary choices. As research continues to unravel the exact relationship between mental health and diet, it’s clear that in the realm of BPD management, what we eat is indeed a significant part of how we feel.
For more on this topic, you might also be interested in our article about how caffeine affects people with BPD.
Sources, Resources, and Further Reading
- Brain glucose metabolism in borderline personality disorder: https://pubmed.ncbi.nlm.nih.gov/9368195/
- How Important is a Healthy Diet for People with Borderline Personality Disorder?: https://clearviewtreatment.com/resources/blog/how-important-is-a-healthy-diet-for-people-with-borderline-personality-disorder/
- Sugar and the Brain: https://hms.harvard.edu/news-events/publications-archive/brain/sugar-brain
- 3 Ways Sugar Impacts Mental Health: https://www.ableto.com/resources/3-ways-sugar-impacts-mental-health/
- 10 Ways To Give Up Sugar: https://www.health.com/nutrition/9-ways-to-quit-sugar-for-good