Mentalization-Based Therapy (MBT) is a type of therapy designed to help people understand and interpret their thoughts and feelings and those of others. It is based on the concept of mentalization, which refers to the ability to understand mental states, such as beliefs, desires, feelings, and attitudes, that underlie overt behaviors. This ability is crucial for self-regulation, secure attachments, and effective interpersonal interactions.
MBT was initially developed by Anthony Bateman and Peter Fonagy for the treatment of Borderline Personality Disorder (BPD), a condition characterized by emotional instability, intense interpersonal relationships, and self-image issues. It has since been applied to other mental health issues, including depression and eating disorders, due to its focus on helping those with problems regulating their emotions and maintaining health interpersonal relationships.
The therapy typically involves both individual and group sessions where therapists help clients explore their mental states and those of others in a safe and supportive environment. Through this process, clients learn to identify and understand their thoughts and feelings before reacting, leading to more adaptive coping strategies and improved relationships. The ultimate goal of MBT is to enhance the person’s capacity to mentalize, particularly during times of emotional stress, thus reducing symptoms and improving overall functioning.
Mentalization
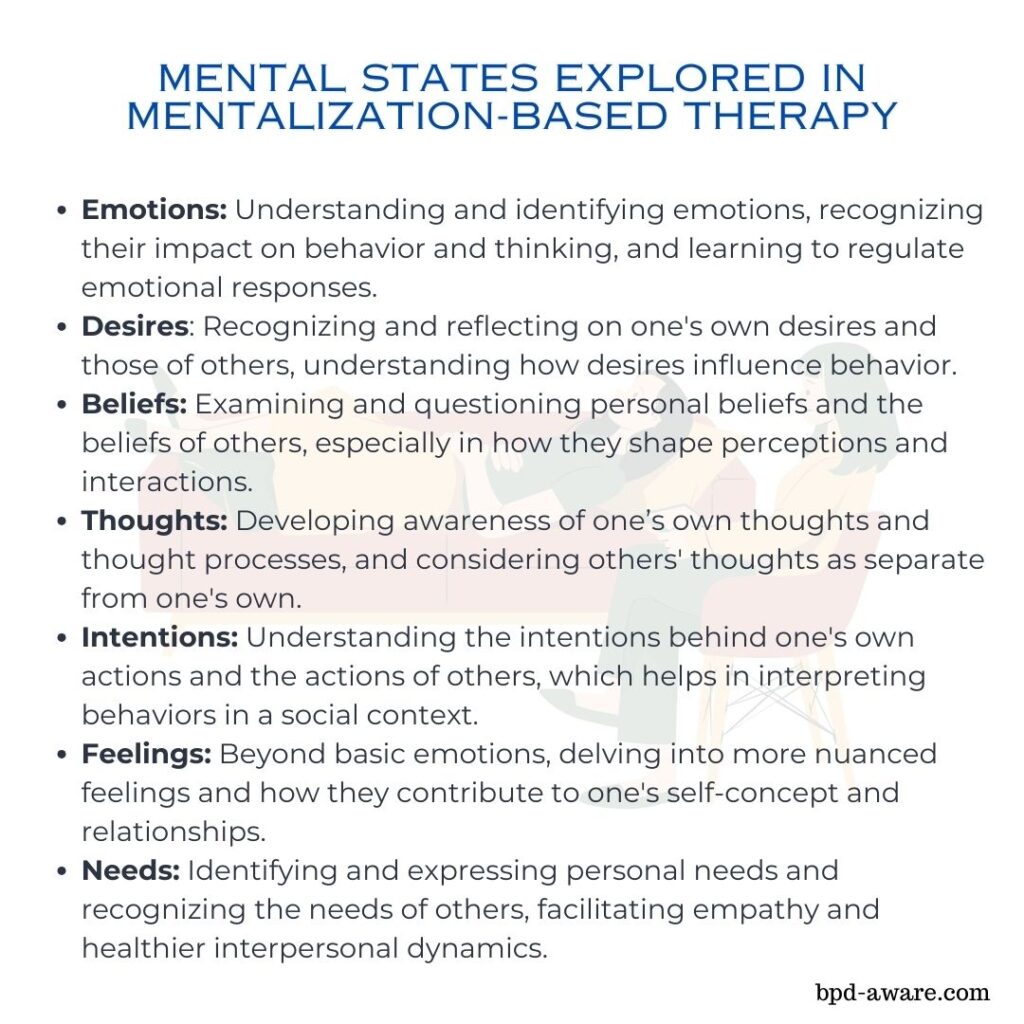
Mentalization refers to the psychological process by which we interpret and make sense of our internal states and those of others. This involves understanding that behaviors and outward expressions are driven by underlying thoughts, feelings, intentions, and desires. Mentalization is a critical aspect of human social interaction, as it enables empathy, helps navigate social complexities, and fosters meaningful relationships.
Mentalization involves several key components:
1. Self-awareness: Recognizing one’s own emotions, thoughts, and motivations.
2. Understanding Others: Inferring the mental states of others based on their behavior, expressions, and context.
3. Perspective-taking: The ability to consider different points of view and understand that others may have thoughts and feelings different from one’s own.
4. Emotional Regulation: Using insights from mentalization to manage and react to emotions in a healthy manner.
5. Attachment Security: Developing healthier and more secure relationships through better understanding and empathy.
In people with conditions like BPD, this capacity to mentalize can be compromised, particularly during times of emotional stress. This can lead to misunderstandings, intense emotional reactions, and problematic interpersonal relationships. MBT aims to strengthen the mentalization process, helping individuals better understand themselves and others, manage their emotions more effectively, and improve their relationships and social functioning. Through therapeutic interventions, clients are encouraged to explore their mental states and those of others in a reflective and curious manner, thereby enhancing their mentalization capacity.
Techniques Used in MBT
Mentalization-Based Therapy employs a variety of techniques aimed at enhancing the patient’s ability to mentalize, particularly in the context of emotional relationships and interactions. These techniques are designed to foster a better understanding of oneself and others, improve emotional regulation, and enhance interpersonal relationships. Here are some of the key techniques and approaches used in MBT:
1. Exploration of Mental States: Therapists encourage clients to explore and reflect upon their mental states and those of others. This involves discussing thoughts, feelings, beliefs, and desires, and considering how these internal states might influence behavior.
2. Promotion of Curiosity: Therapists foster a sense of curiosity in clients about their own and others’ mental states. This helps in developing a more nuanced understanding of why people act the way they do, leading to greater empathy and improved relationships.
3. Linking Mental States to Actions: Clients are helped to make connections between their thoughts, feelings, and behaviors. This can increase their awareness of how their internal states influence their actions and the outcomes of those actions.
4. Identification of Affective States: Therapists assist clients in identifying and labeling their emotions. Recognizing and naming emotions is a crucial step in learning how to regulate them effectively.
5. Mindfulness Techniques: Mindfulness practices may be incorporated to enhance self-awareness and present-moment focus. These techniques can help individuals become more cognizant of their mental states without immediately reacting to them.
6. Use of the Therapeutic Relationship: The relationship between the therapist and the client serves as a guide for healthy interpersonal interaction. Therapists use moments of misunderstanding or conflict within the therapy as opportunities to practice mentalization, thereby improving the client’s skills in real time.
7. Group Therapy: Group sessions provide a dynamic environment where clients can practice mentalization with peers. These sessions allow for the exploration of different perspectives, the practice of empathy, and the observation of social interactions in a controlled setting.
8. Psychoeducation: Clients receive education about mentalization and its importance in emotional regulation and interpersonal relationships. Understanding the concept can motivate clients to engage more deeply with the therapeutic process.
9. Homework Assignments: Clients may be given exercises to practice mentalization outside of therapy sessions. These could include reflective writing, practicing mindfulness, or engaging in specific social interactions with mentalization in mind.
The specific techniques used in MBT can vary depending on the individual’s needs and the setting of the therapy (e.g., individual vs. group therapy). The end goal is to create an environment that supports and enhances the client’s ability to understand and interpret mental states in a way that promotes emotional well-being and healthier relationships.
The Process
The process of Mentalization-Based Therapy for treating BPD is structured to enhance the patient’s ability to mentalize, especially in the context of emotional relationships. This therapeutic approach is designed to improve emotional regulation, interpersonal relationships, and self-understanding. The MBT process typically involves several key stages and components:
Assessment Phase
- Initial Assessment: The process starts with an assessment of the individual’s psychological state, history, and symptoms to confirm the diagnosis of BPD and establish a baseline for therapy.
- Orientation to MBT: Patients are introduced to the concept of mentalization, the goals of MBT, and how the therapy process works.
Treatment Phases
MBT can be divided into two main phases:
The Initial Phase focuses on building a therapeutic alliance, developing a shared understanding of the patient’s difficulties in terms of mentalization failures, and setting treatment goals.
The Main Body of Treatment involves the core work of MBT, which includes:
- Enhancing Mentalization Capacity: Through individual and group therapy sessions, therapists help patients focus on current mental states, emphasizing curiosity and exploration of feelings, thoughts, and beliefs.
- Identifying and Exploring Triggers: Patients learn to identify specific situations or relationships that trigger mentalization breakdowns, leading to emotional dysregulation or interpersonal difficulties.
- Addressing Breakdowns in Mentalization: Therapy sessions aim to address and repair instances where the patient’s ability to mentalize breaks down, particularly focusing on moments of high emotional arousal.
- Linking Past and Present: Therapists help patients explore how past experiences influence current mental states and relationships, fostering a deeper understanding of their emotional patterns.
Specific Techniques
- Reflective Functioning: Therapists encourage patients to reflect on their thoughts and feelings and those of others, promoting greater empathy and understanding.
- Therapeutic Stance: Therapists maintain a stance of not-knowing and curiosity, facilitating a safe environment for exploration and discovery.
- Use of the Therapeutic Relationship: The relationship between the therapist and the patient is used as a real-time tool for enhancing mentalization, with therapists highlighting moments of misunderstanding or misinterpretation as opportunities for learning.
- Group Therapy: Provides a platform for patients to practice mentalization with others, offering feedback and perspective-taking in a controlled setting.
Termination Phase
- Consolidation of Gains: As therapy concludes, efforts are made to consolidate the skills and insights gained during treatment, ensuring the patient can maintain their mentalization capacity outside of the therapeutic context.
- Planning for the Future: Therapists and patients work together to develop strategies for managing future stressors and triggers, reinforcing the use of mentalization in everyday life.
Follow-Up and Maintenance
- Ongoing Support: Some MBT programs offer follow-up sessions or booster sessions. These sessions reinforce the skills learned during therapy and provide ongoing support.
Throughout the MBT process for BPD, the emphasis is on creating a therapeutic environment that promotes growth, understanding, and resilience, equipping patients with the tools they need to regulate their emotions, improve their relationships, and lead more fulfilling lives.
Pros of Mentalization-Based Therapy
1. Improves Emotional Regulation: MBT helps individuals better understand and manage their emotions. This new understanding can lead to decreased impulsivity and more adaptive responses to stress.
2. Enhances Interpersonal Relationships: By improving understanding of oneself and others, MBT can lead to healthier, more secure relationships and reduce interpersonal conflicts.
3. Broad Application: Although initially developed for BPD, MBT has been adapted for other mental health issues, including depression, eating disorders, and trauma-related conditions, showing its flexibility and broad applicability.
4. Fosters Self-Reflection: MBT encourages ongoing self-reflection and curiosity about mental states, which can contribute to personal growth and increased self-awareness over time.
5. Evidence-Based: MBT is supported by research evidence, particularly for BPD, demonstrating its effectiveness in reducing symptoms and improving functioning.
6. Group and Individual Formats: MBT can be provided in both individual and group therapy settings, providing flexibility and the opportunity to practice mentalization skills in different social contexts.
Cons of Mentalization-Based Therapy
1. Requires High Level of Therapist Training: Effective delivery of MBT necessitates therapists to have specialized training and skills in mentalization techniques, which can limit access to qualified providers.
2. Time-Intensive: MBT typically requires a significant time commitment, with therapy often spanning several months to years, which might not be feasible for all clients.
3. Complexity for Clients: Some individuals may find the concept of mentalization difficult to grasp initially, potentially affecting their engagement with the therapy process.
4. Limited Research on Long-Term Outcomes: While there is strong evidence supporting MBT’s effectiveness in the short to medium term, more research is needed to fully understand its long-term outcomes.
5. Potential for Over-Emphasis on Mentalization: In some cases, there might be an over-focus on mentalization at the expense of addressing other important factors or symptoms not directly related to mentalizing abilities.
6. Accessibility: Access to MBT can be limited by geographical location, availability of trained therapists, and cost, which may make it difficult for some individuals to receive this type of therapy.
Effectiveness of Mentalization-Based Therapy
In one study into Mentalization-Based Therapy, researchers evaluated its efficacy within a partial hospital setting compared to standard psychiatric care for individuals with Borderline Personality Disorder. This study was conducted in a conventional clinical environment, with mental health practitioners who lacked comprehensive psychotherapy training but received supervision from experts. The findings revealed that participants in the partial hospital program experienced significant improvements across all evaluated metrics, unlike the control group, which saw minimal to no progress or even worsened during the study period. Enhancements in symptoms of depression, reductions in suicidal behavior and self-harm, fewer hospital admissions, and improvements in social and interpersonal skills were observed starting from six months, continuing up to the 18-month treatment conclusion.
The 44 participants from the initial study were followed up at three-month intervals post-trial, utilizing the same set of outcome measures. This follow-up demonstrated that those who underwent treatment in the partial hospital setting not only preserved their significant progress but also exhibited ongoing significant enhancements in most areas assessed, unlike the control group, which only showed negligible changes. The sustained and continued improvements, especially in social and interpersonal functioning, indicate that the treatment may have initiated long-term rehabilitative effects.
Final Thoughts
The essence of MBT lies in its ability to help the individual develop a deeper understanding of themself and others, thereby addressing the core challenges faced by those with BPD, including emotional dysregulation, impulsivity, and turbulent relationships. Through its structured yet flexible framework, MBT equips people with the tools necessary to traverse the complex landscape of their emotions and relationships, promoting healing and growth.
MBT’s emphasis on building mentalization capacity offers a pathway to more stable and fulfilling interpersonal relationships, contributing to a higher quality of life for those affected. The therapy’s focus on understanding and interpreting mental states fosters a sense of empathy and connection, core elements that are often compromised in BPD.
However, the journey through MBT requires commitment from both the therapist and the patient, a testament to the collaborative nature of this therapeutic approach. It is a process that necessitates patience, openness, and a willingness to explore the depths of one’s emotional and mental experiences. The challenges inherent in this process are paralleled by its profound potential for transformation and healing.
As we explore and refine therapeutic approaches for BPD, MBT stands out as a pivotal intervention that aligns closely with the lived experiences of those it seeks to help. Its capacity to engender meaningful change by enhancing mentalization offers a valuable perspective in the ongoing quest to understand and treat BPD effectively. Ultimately, MBT represents a significant stride forward in the treatment of BPD, promising a future where individuals can navigate their worlds with greater clarity, stability, and hope.
Sources, Resources, And Further Reading
- What is Mentalization-Based Therapy?: https://www.psychologytoday.com/us/therapy-types/mentalization-based-therapy
- When is MBT used?: https://www.healthline.com/health/mentalization-based-therapy#mbt
- Mentalization Based Therapy for BPD https://www.verywellmind.com/mentalization-therapy-for-bpd-425459
- Mentalization-Based Treatment: A Common-Sense Approach to Borderline Personality Disorder: https://www.psychiatrictimes.com/view/mentalization-based-treatment-common-sense-approach-borderline-personality-disorder
- Mentalization based treatment for borderline personality disorder: https://pmc.ncbi.nlm.nih.gov/articles/PMC2816926/