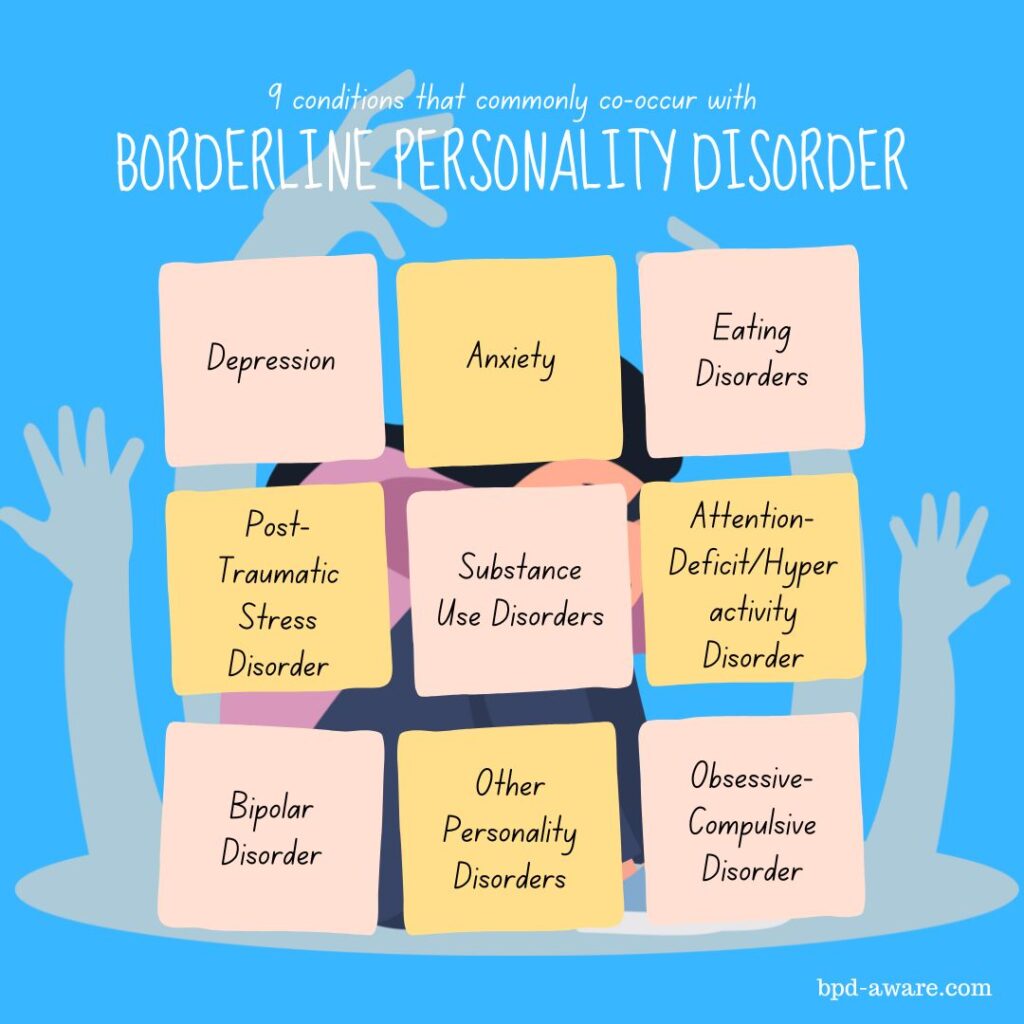
Borderline Personality Disorder (BPD) is very challenging to live with. What makes it even tougher is that BPD often co-occurs with other mental health conditions, something that’s referred to as a comorbidity.
Comorbidities add an extra level of difficulty to getting a proper diagnosis and the correct treatment. Of course, they also make the day-to-day lives of the sufferer that much harder. Some of the comorbidities are quite common among the general population, but others are particularly prevalent in people with BPD.
It’s important to note that not everyone with BPD necessarily has a co-occurring condition, while others may have several. And, like BPD, each condition can manifest itself in a multitude of ways, making the scope of someone’s mental health incredibly complex. It should also be noted that the following list of conditions is by no means exhaustive or exclusive.
Depression
Major Depressive Episodes (MDE) often co-occur alongside BPD. Around 70% to 80% of people with BPD will experience at least one MDE (compared to 21% of people without BPD) MDEs throughout their life. In some cases, depression may be seen as merely a symptom of BPD; in other cases, it may warrant its own diagnosis.
Depression is typically treated with medication and, in severe cases, therapy. When depression co-occurs with BPD, it can lead to a worsening of all the usual symptoms of BPD that the individual suffers from. For example, depression can make emotional regulation much more difficult, leading to increased mood swings, irritability, and rage.
Anxiety
Anxiety disorders are also very common in people with BPD, with comorbidity rates as high as 90%. Anxiety rates in the general population are just over 30%. Much like depression, anxiety may be seen as a symptom of BPD in some cases; and warrants its own diagnosis in others.
Anxiety is treated with medication in most cases, and occasionally therapy. BPD symptoms such as the fear of abandonment, unstable self-image, and emotional dysregulation can all be made worse because of anxiety.
Evidence shows that people with BPD often have a hyperactive amygdala and hippocampus – two parts of the brain that work together to assess threats. This means that those with BPD are often in the fight-or-flight mode and in a constant state of anxiety.
Bipolar Disorder
Bipolar Disorder and Borderline Personality Disorder share overlapping symptoms such as mood instability, impulsivity, and emotional dysregulation. This can lead to misdiagnosis and people receiving the wrong treatment. One of the key differences is that Bipolar episodes generally last longer and are less tied to external stimuli.
However, it’s entirely possible to have both BPD and Bipolar Disorder at the same time, something referred to colloquially as Borderpolar. The co-occurrence of these two disorders can lead to severe impairment which requires nuanced treatment.
Click here to read more about BPD and Bipolar Disorder.
Post-Traumatic Stress Disorder (PTSD)
PTSD can occur after someone has experienced a traumatic event such as a physical or sexual assault or emotional abuse. Someone with PTSD may experience a wide range of symptoms such as avoidance of social situations, intrusive thoughts, flashbacks, self-blame, guilt, shame, a heightened sense of alertness, and insomnia.
Studies have found that many people with BPD have suffered from trauma which may have triggered their personality disorder in the first place. There are also several similarities in both the physical and chemical states of the brains of people with BPD and PTSD.
A study in 2010 reported that 32% of people with BPD also met the criteria to be diagnosed with PTSD.
Eating Disorders
Over half of people with BPD meet the criteria for an Eating Disorder, according to one study. When you have an unhealthy relationship with food, it can affect you in many ways. You’re likely not receiving the nutrients your body and mind need to be your best. In people with BPD, this can cause a significant worsening of symptoms.
It’s thought that the key link between BPD and Eating Disorders is the unstable sense of self-image many people with BPD suffer from. Eating Disorders can also be a maladaptive behavior employed to give the individual a false sense of control. The individual may believe they’re in control of what they’re putting (or not putting) into their body when, in reality, the Eating Disorder is controlling them.
Treatment for BPD and Eating Disorders is typically done separately.
Click here to read our article about the link between BPD and Eating Disorders.
Substance Use Disorders
The link between Borderline Personality Disorder and substance abuse is a strong one. Many people with BPD have issues with impulse control as well as self-destructive tendencies. Combine these with the day-to-day struggles of living with BPD and you have a recipe for substance abuse issues.
Other factors that can lead to substance abuse issues include instability in relationships, emotional dysregulation, trauma, and genetic factors.
The most commonly abused substances are alcohol, cocaine, opioids, and cannabis. Prescribed medication, particularly anti-anxiety medication, can also be abused. Poly-substance abuse (the use of two or more illicit substances) is also frequent among people with BPD.
Depending on the scale of the substance abuse, this may be tackled with BPD therapy or require a secondary therapeutic option.
Attention-Deficit/Hyperactivity Disorder (ADHD)
BPD and ADHD frequently co-occur, several studies have found much higher rates of ADHD in people with BPD and vice versa. One Swedish study found that individuals with ADHD are 19.4 times more likely to be diagnosed with BPD than those without ADHD.
Both conditions involve significant challenges with impulsivity, as well as issues with concentration and emotional dysregulation. People with both BPD and ADHD can find it nigh-on impossible to control certain impulses, which can lead to self-destructive and dangerous decision-making.
BPD and ADHD also share remarkable similarities in dysfunctional areas of the brain related to executive functioning, emotional regulation, and, again, impulse control.
ADHD is typically treated with medication, while BPD is usually treated with therapy. People with both conditions benefit greatly from receiving the proper treatment.
Obsessive-Compulsive Disorder (OCD)
Research suggests that roughly 20% of people with BPD also have OCD. OCD is a condition characterized by unwanted thoughts (obsessions) and repetitive actions (compulsions) which are performed to relieve the stress caused by the obsessions.
One study found that the rate of comorbidity between BPD and OCD is three times higher than within the general population.
These two conditions can negatively feed on each other. For example, OCD may lead to self-harming behaviors, which are made worse by the mood swings of BPD.
Other Personality Disorders
Sadly, having Borderline Personality Disorder doesn’t protect you from having other personality disorders. Having multiple personality disorders within the same cluster is rather common. In the case of BPD, and Cluster B personality disorders, that means comorbidity with Narcissistic Personality Disorder, Antisocial Personality Disorder, and Histrionic Personality Disorder. It’s also possible to have, for example, Borderline Personality Disorder (Cluster B) and Schizoid Personality Disorder (BPD).
Living with one personality is hard enough, especially when it comes to BPD, but adding another personality disorder to this mix makes life tough beyond belief. The rates of comorbidity vary quite wildly from study to study, with some stating as low as 17% while others state as high as 80%. Even at the lowest figure, this is still twice as high as within the general population.
Having comorbid personality disorders can make receiving the correct diagnosis very difficult, as well as receiving the proper treatment.
Final Thoughts
Living with Borderline Personality Disorder is a roller coaster at the best of times. At the worst of times, it feels like a never-ending abyss. When you couple that with one or more comorbid conditions, it makes everything so much harder.
If you’re reading this because you have BPD and believe you may have a co-occurring condition, we urge you to seek professional advice as soon as possible. Even if you’re already undergoing treatment for BPD, working on other troubling areas will be mutually beneficial to both conditions.
We also urge those reading who don’t have BPD to realize there’s so much more to an individual than just a label. No person is just one thing or has just one problem. We are all made up of so many passions, joys, problems, and hardships.
Kindness and empathy go a long way.
Sources, Resources, and Further Reading
- Comorbidities in Borderline Personality Disorder: https://www.psychiatrictimes.com/view/comorbidities-borderline-personality-disorder
- 7 Mental Health Conditions That Occur With Borderline Personality Disorder: https://www.everydayhealth.com/bpd/borderline-personality-disorder-something-else-mental-conditions-occur-bpd/
- BPD and co-occurring disorders: https://www.borderlineintheact.org.au/living-with-bpd/bpd-comorbidities/
- We don’t talk much about comorbidity here: https://www.reddit.com/r/BPD/comments/r6po11/we_dont_talk_much_about_comorbidity_here/