Borderline Personality Disorder (BPD) is a mental health disorder that is in the Cluster B of personality disorders. It’s characterized by a pervasive pattern of instability in interpersonal relationships, self-image, and emotions, as well as marked impulsivity.
The nine major signs of BPD are:
- Emotional Instability: Individuals with BPD often experience intense and fluctuating emotions. They may feel happy and content one moment and extremely upset or distressed the next. These mood swings can be rapid and are often triggered by interpersonal stresses.
- Unstable Relationships: People with BPD typically have a pattern of intense and unstable relationships. They might idealize someone at the start of a relationship, but then suddenly shift to devaluing them. This pattern stems from an intense fear of abandonment and an inability to maintain stable and realistic views of others.
- Disturbed Self-Image: A person with BPD might have a significantly distorted sense of self. They can struggle with identity issues, often showing signs of a shifting self-image, uncertain about their values, goals, or loyalties.
- Impulsivity: Individuals with BPD often engage in impulsive and risky behaviors. This can include reckless driving, substance abuse, binge eating, or risky sexual behaviors. Such actions are often driven by immediate gratification without consideration of the consequences.
- Fear of Abandonment: One of the hallmarks of BPD is an intense fear of abandonment or being rejected. Even a brief separation or a change in plans can trigger intense fear or anger.
- Intense Anger: People with BPD may display disproportionately intense anger or struggle to control their anger. This can manifest as temper outbursts, physical fights, or ongoing resentment.
- Self-Harm and Suicidal Behavior: Self-harming behaviors, such as cutting, and suicidal threats or attempts are not uncommon in people with BPD.
- Chronic Feelings of Emptiness: Individuals with BPD often state the feel empty inside, as if there is a void or a hole within them.
- Dissociation or Paranoia: Under stress, people with BPD may experience paranoid thoughts or dissociative symptoms (feeling cut off from oneself or reality).
Someone with five or more of these symptoms is considered to have BPD.
Borderline Personality Disorder is usually diagnosed in late adolescence or early adulthood and can be effectively treated with therapy, medication, or a combination of both. Therapy approaches like Dialectical Behavior Therapy (DBT), Schema Therapy (ST), and Transference-Focused Psychotherapy (TFP) have been found particularly effective.
Background of Transference-Focused Psychotherapy
Developed by Otto Kernberg and his colleagues in the late 20th century, TFP is rooted in object relations theory. This theory suggests that individuals internalize early relationships with significant others, which then influence their adult interactions and self-perception. TFP evolved as a structured, twice-weekly therapy specifically designed for individuals with BPD and other severe personality disorders.
The Goals of Transference-Focused Psychotherapy
TFP is specifically tailored to treat individuals with Borderline Personality Disorder and other personality disorders like Antisocial Personality Disorder. The primary goals of TFP in the context of BPD are multifaceted, focusing on improving emotional, cognitive, and interpersonal functioning. These goals include:
Integrating Split Representations: One of the main objectives is to help patients integrate split-off parts of their perceptions about themselves and others. In BPD, individuals often oscillate between extreme, polarized views of themselves and others (e.g., all good or all bad). TFP aims to help them see themselves and others in a more integrated, realistic, and nuanced way.
Improving Emotional Regulation: TFP helps patients understand and manage their intense emotional reactions. By working through the transference relationship (how feelings about significant others are projected onto the therapist), patients learn to identify their emotions and regulate them more effectively.
Enhancing Interpersonal Relationships: The therapy focuses on improving interpersonal functioning. By exploring relationships within the therapy setting, patients gain insights into their relationship patterns, which can lead to healthier and more stable relationships outside of therapy.
Reducing Self-Destructive Behaviors: TFP aims to decrease self-harm and suicidal behaviors, which are common in individuals with BPD. Through the therapeutic process, patients learn alternative ways to cope with intense emotions and situations without resorting to self-destructive behavior.
Building a Stable Sense of Self: TFP works to help patients develop a more coherent and stable sense of self. This includes addressing issues of identity and self-worth, which are often unstable in BPD.
Reducing Dependency on Defense Mechanisms: The therapy aims to help patients recognize and reduce reliance on maladaptive defense mechanisms, such as splitting, idealization, and devaluation, which can interfere with their perception of reality and relationships.
Resolving Internal Conflicts: TFP assists in identifying and resolving internal conflicts, particularly those that are unconsciously played out in the transference relationship with the therapist.
Enhancing Reality Testing: The therapy improves the patient’s ability to differentiate between thoughts and feelings that are internally generated and those that are based on external reality.
By achieving these goals, TFP aims to bring about significant changes in the patient’s overall personality structure, leading to better functioning and an improved quality of life. The process is intensive and requires a strong commitment from both the patient and the therapist, but it can be highly effective for those struggling with BPD.
The Process
The therapeutic process in Transference-Focused Psychotherapy for treating Borderline Personality Disorder is structured and intensive, typically involving two sessions per week. This process is designed to address the complex dynamics of BPD and involves several key stages:
Initial Phase: Assessment and Contract Setting
Assessment: TFP begins with a thorough assessment phase, where the therapist gains an understanding of the patient’s history, symptoms, and current functioning. This includes exploring the patient’s relationships, emotional experiences, self-image, and behaviors.
Treatment Contract: A unique feature of TFP is the establishment of a treatment contract. This contract sets the framework for therapy, including goals, responsibilities, and boundaries. It also addresses safety issues, particularly concerning self-harm and suicidal behaviors.
Early Phase: Establishing the Therapeutic Relationship and Identifying Patterns
Developing the Therapeutic Alliance: Building a strong therapeutic alliance is crucial. The therapist and patient work together to establish a relationship based on trust and understanding.
Identifying Transference Patterns: Early sessions focus on identifying and exploring transference patterns – how feelings and thoughts about significant others are projected onto the therapist. These patterns reflect the patient’s internal world and offer a window into their relational dynamics.
Middle Phase: Exploration and Interpretation
Clarification and Confrontation: The therapist helps the patient to clarify their thoughts and feelings, and confronts discrepancies and distortions in their perceptions and narratives.
Working Through Transference: A significant part of TFP involves working through the transference relationship. The therapist helps the client recognize how past experiences influence current perceptions and behaviors.
Addressing Splitting and Integration: The therapy focuses on integrating the split-off or polarized views (idealizing vs. devaluing) of self and others, helping the patient to develop a more nuanced and realistic self-image and view of others.
Later Phase: Integration and Resolution
Integrating Insights: In this phase, insights and changes are consolidated. The patient works on integrating the different aspects of their personality into a more cohesive whole.
Applying Changes to Outside Relationships: The patient applies the insights and skills learned in therapy to their relationships outside of the therapeutic setting.
Preparing for Termination: The ending of therapy is carefully managed. Issues related to dependency, loss, and autonomy are addressed.
Termination Phase
Reviewing Progress: The therapist and patient review the progress made during therapy.
Addressing Endings: The termination process itself is used therapeutically to address feelings about endings and separations, which are often challenging for individuals with BPD.
Throughout the process, TFP requires a high level of engagement from both the therapist and the patient. The therapist remains active and interpretative, focusing on the here-and-now of the therapeutic relationship to gain insight into the patient’s broader relational patterns and internal world. This process can be mentally and emotionally challenging, but it is designed to bring about significant changes in the patient’s personality structure and overall functioning.
Exercises Used in Transference-Focused Psychotherapy
Transference-Focused Psychotherapy primarily involves conversational techniques and interpretive strategies, rather than structured exercises like those found in other therapeutic approaches. The focus is on the dynamic interaction between the therapist and the patient, particularly as it pertains to the exploration of the transference relationship. Key techniques or “exercises” used in TFP include:
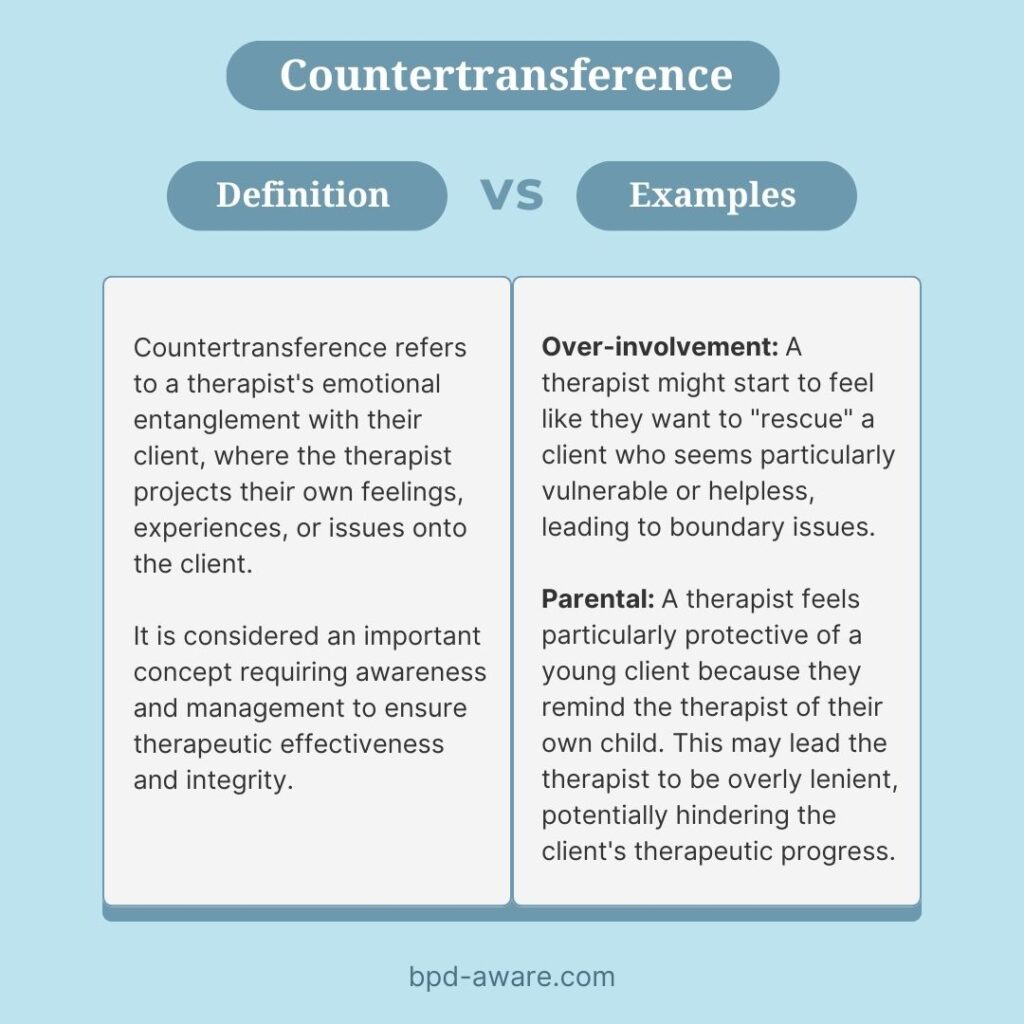
Interpretation of Transference and Countertransference:
The therapist interprets how the patient’s feelings, thoughts, and behaviors towards the therapist (transference) reflect their experiences with significant others in their past. Simultaneously, the therapist’s emotional responses to the patient (countertransference) are used as a tool for understanding the patient’s internal world.
Exploration of Defense Mechanisms:
This involves identifying and discussing the defense mechanisms the patient uses to avoid distressing thoughts and feelings. For example, a patient might use denial or projection as a way to cope with painful emotions, and these defenses are explored and interpreted in the therapy sessions.
Identification and Discussion of Splitting:
Splitting is a common defense mechanism in BPD where a person’s view of themselves and others shifts between extremes. The therapist help the patient identify instances of splitting and to explore more integrated and nuanced views of self and others.
Confrontation of Distorted Perceptions and Beliefs:
The therapist gently confronts inconsistencies and distortions in the patient’s narratives and perceptions. This helps the patient to recognize and reconsider these distortions.
Clarification of Thoughts and Feelings:
The therapist helps the patient clarify complex or confusing emotions and thoughts. This can involve breaking down overwhelming experiences into more manageable parts for discussion and understanding.
Linking Past and Present:
The therapist and patient work together to understand how past experiences influence current behaviors and feelings. This often involves linking childhood experiences to present-day relationship patterns.
Working Through Emotional Pain and Trauma:
This involves helping the patient to confront and process painful emotions and traumatic experiences, rather than avoiding or acting them out.
Building a Narrative:
The therapist aids the patient in developing a coherent life narrative, integrating fragmented memories and experiences into a more cohesive story.
It’s important to note that these techniques are not exercises in the traditional sense, but rather integral parts of the therapeutic conversation and process. They are used flexibly and tailored to the needs and progress of the patient. The aim is to develop greater self-understanding and healthier ways of relating to the self and others.
What is the success rate of Transference-Focused Psychotherapy for Borderline Personality Disorder?
The success rate of Transference-Focused Psychotherapy in treating Borderline Personality Disorder is an area of ongoing research, and like all psychotherapeutic treatments, its effectiveness can vary based on numerous factors including patient characteristics, therapist skill, and the specific nature of the disorder. However, several studies have provided encouraging results regarding the efficacy of TFP for BPD.
One study by Josephine Giesen-Bloo, MSc; Richard van Dyck, MD, PhD; Philip Spinhoven, PhD; et al found Transference-Focused Psychotherapy to be as successful in reducing symptoms of BPD as Schema Therapy. However, TFP has a higher attrition rate than ST, meaning that more patients dropped out of TFP treatment.
Final Thoughts
TFP’s strengths lie in its structured approach and depth of exploration into the patient’s internal world, fostering insights that can lead to significant personal growth and stability. However, it is important to acknowledge that the success of TFP, like any therapeutic intervention, depends on various factors including patient engagement, the severity of the disorder, and the skill of the therapist. It is not a quick fix, nor is it the right fit for everyone. The journey through TFP can be challenging and requires a significant commitment of time and emotional energy from both the patient and the therapist.
In the broader context of BPD treatment, TFP stands alongside other effective therapies such as Dialectical Behavior Therapy and Schema Therapy, each with its unique strengths and approaches. The choice of therapy should be tailored to the individual needs of the patient, considering their specific symptoms, circumstances, and treatment goals.
Ultimately, the growing body of research and clinical experience surrounding TFP offers valuable insights and hope for those affected by BPD. While not a panacea, TFP is a significant tool in the therapeutic arsenal, offering a pathway to greater emotional stability and improved interpersonal relationships for many individuals with BPD.S
Sources, Resources, and Further Reading
- Understanding Transference-Focused Psychotherapy: https://www.mcleanhospital.org/essential/tfp
- DBT vs Transference-Focused Psychotherapy?: https://www.reddit.com/r/therapists/comments/12eg434/dbt_vs_transferencefocused_psychotherapy/
- Outpatient Psychotherapy for Borderline Personality Disorder: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209673