Therapy is a vital tool for people managing the challenge of living with Borderline Personality Disorder (BPD), but what happens when you start to doubt whether your therapist is helping you effectively? Recognizing signs that your therapist might be wrong is crucial for ensuring you receive the support and guidance you need.
In this article, we’ll explore what kinds of mistakes therapists can make, how to confront your therapist constructively, the importance of how they deal with being challenged, and when to consider switching to a new therapist.
Mistakes Therapists Make
Therapists are viewed as possessing superior judgment and reasoning. However, therapists, like anyone else, are human and prone to making mistakes. When therapists make a mistake, it can disrupt this idealization and diminish the patient’s trust in their capabilities. While some forms of therapy can weather the storm of therapist errors and may even grow stronger from them, others may falter depending on the error’s nature and the therapist’s response.
Here are the three kinds of errors therapists can make:
Factual Errors
Some typical factual errors include:
- Forgetting details the patient has shared in the past.
- Providing factually incorrect information.
- Neglecting to follow through on something they promised.
Acknowledging these errors typically allows the therapy to proceed unaffected. For certain patients, seeing their therapist admit to a mistake and apologize can be a constructive experience, bolstering their respect and trust. In a way, it helps to humanize the therapist too. Here is an example of how this might play out:
- Clara mentions a chronic fear of abandonment.
- Dr. Good suggests this might relate to her father having abandoned the family when she was young.
- Clara clarifies that her father never left the family.
- Dr. Good apologizes for the oversight and requests more details about her family background.
In this scenario, Dr. Good demonstrates professionalism by admitting their mistake and asking the patient to share the information again, likely keeping the therapeutic process on track.
Contrast this with Dr. Bad’s approach:
- Clara discusses her chronic fear of abandonment.
- Dr. Bad connects this to her father leaving her at a young age.
- Upon Clara’s correction that her father never left, Dr. Bad insinuates Clara shared this fact earlier.
- Despite Clara’s insistence on having provided this information earlier, Dr. Bad deflects, suggesting Clara’s fear of abandonment stems from family trauma rather than acknowledging their mistake.
In this situation, Clara might feel invalidated by Dr. Bad, who not only refuses to accept the possibility of being wrong but also redirects the issue back onto Clara. This could seriously undermine the therapeutic relationship. The patient will lose trust in the therapist when they appear more focused on being right than helping them.
Mistakes in Understanding
Another common mistake therapists make is getting emotions wrong. Here’s an example where Dr. Good misunderstood Ryan’s feelings.
- Ryan: My father was there physically but he was never emotionally available. He just wasn’t capable of opening up to anyone.
- Dr. Good: You seem angry about that.
- Ryan: I’m not angry, just sad. He grew up in a different time. In a way, I feel sorry for him.
- Dr. Good: I can see how that would make you feel sad.
Here, Dr. Good thought Ryan was mad but quickly saw they were sad instead. This helped them to talk about Ryan’s sadness more openly.
Here’s how Dr. Bad might react in the same situation.
- Ryan: My father was there physically but he was never emotionally available. He just wasn’t capable of opening up to anyone.
- Dr. Bad: You seem angry about that.
- Ryan: I’m not angry, just sad. He grew up in a different time. In a way, I feel sorry for him.
- Dr. Bad: I’m it’s hard to deal with the fact you’re angry at your father.
- Ryan: I’m not angry at him.
- Dr. Bad: You must be angry at him. How could you not be?
Dr. Bad didn’t catch on to Ryan’s sadness. Instead, they made Ryan feel like they didn’t understand their feelings. This is the type of mistake and lack of correction that could make Ryan quit therapy with Dr. Bad and turn them away from therapy altogether.
Mistakes in Diagnosis
It’s hard to pin down a mental health issue. Unlike other health problems that can be checked with tests or scans, mental health depends on spotting behavior patterns. Wrong calls can lead to the wrong help, like following an incorrect treatment plan. Still, a good therapist can fix these mistakes.
- Jennifer: I know you diagnosed me as having Bipolar Disorder but I think it could be Borderline Personality Disorder.
- Dr. Good: You could be right. We could try a different approach and see if that works better for you.
This way, Dr. Good works together with Jennifer to try and find the real problem.
Dr. Bad had a different take.
- Jennifer: I know you diagnosed me as having Bipolar Disorder but I think it could be Borderline Personality Disorder.
- Dr. Bad: It’s clear to me that you have Bipolar Disorder. Discussing it further is a waste of time.
- Jennifer: I’d like a second opinion about this.
- Dr. Bad: I’m sure they’ll tell you the same as I have.
Here, Dr. Bad insists Jennifer has Bipolar Disorder and should continue treating her issues as such, ignoring her feelings and concerns.
Even the best therapists make mistakes at times. It’s often how they react and correct their position that can differentiate a good therapist from a bad one.
Signs a Therapist Might Not Be Right For You
You feel misunderstood or invalidated: Therapy aims to be a judgment-free zone where you can express your thoughts and feelings freely. Yet, if you often find yourself feeling misunderstood or invalidated by your therapist, it might obstruct your journey toward healing. Indicators of feeling not understood include:
- Your experiences are dismissed or belittled by your therapist.
- They appear uninterested or easily distracted during your discussions.
- You’re hesitant to share information, fearing judgment.
- Your therapist makes unfounded assumptions about what you’re thinking or feeling without truly grasping your viewpoint.
Discrepancies between therapeutic goals and personal values: In therapy, setting goals is a mutual activity, intended to reflect both your aspirations and your values. If you discover that your therapist’s goals for your sessions clash with your personal beliefs, it can lead to discomfort and impede progress. Signs of this misalignment might include:
- Being encouraged to act in ways that go against your principles.
- Feeling coerced into a therapeutic approach that doesn’t feel right for you.
- Sensing that your therapist is placing their objectives above your needs and preferences.
- Feeling guilty or uneasy when trying to follow through on your therapist’s suggestions.
Stagnation or deterioration in therapy: If you’re not seeing any improvement or, if your symptoms have intensified while in therapy, it’s a significant sign that the current approach might not be the right fit. Therapy is supposed to be a path to improvement, and while it’s often a complex process, you shouldn’t be consistently feeling stuck or regressing. Signs of this issue include:
- Persistent struggles with the same problems without noticing improvements.
- Your symptoms are becoming worse, or new ones are appearing despite engaging in therapy.
- Your therapist does not alter their strategy or treatment plan even though you’re not making progress.
- Feeling hopeless or pessimistic about the benefits of continuing therapy.
Persistent unease or mistrust in the therapeutic relationship: A successful therapeutic relationship is grounded in trust and a strong connection with your therapist. If you constantly feel uneasy or mistrustful towards your therapist, it could be a red flag indicating deeper issues. Indicators of persistent unease or mistrust include:
- Reluctance to be open or vulnerable with your therapist.
- Doubting the intentions or the advice provided by your therapist.
- Feeling anxious or unsettled before or during therapy sessions.
- An instinctual feeling that something in the therapeutic relationship isn’t right.
Knowing when your therapist may be wrong is key to looking out for yourself and getting the help you need. Trust your gut and don’t hesitate to speak up if something feels off in your therapy. Therapy should boost you up, and it’s fine to find a new therapist if the one you have now isn’t working out. Recovering from BPD is important, and you deserve the best help you can get.
Steps to Take When You Disagree with Your Therapist
When you don’t see eye to eye with your therapist, for whatever reason, it’s best to handle it with care and clarity. Here are steps to take if you disagree with your therapist:
Think about how you feel and accept those feelings: Start by thinking over your feelings and thoughts about the problematic issue. Know it’s okay to feel uneasy or unsure in therapy. Reflecting can help you see why you feel and uneasy and what you hope to achieve when discussing the issue with your therapist.
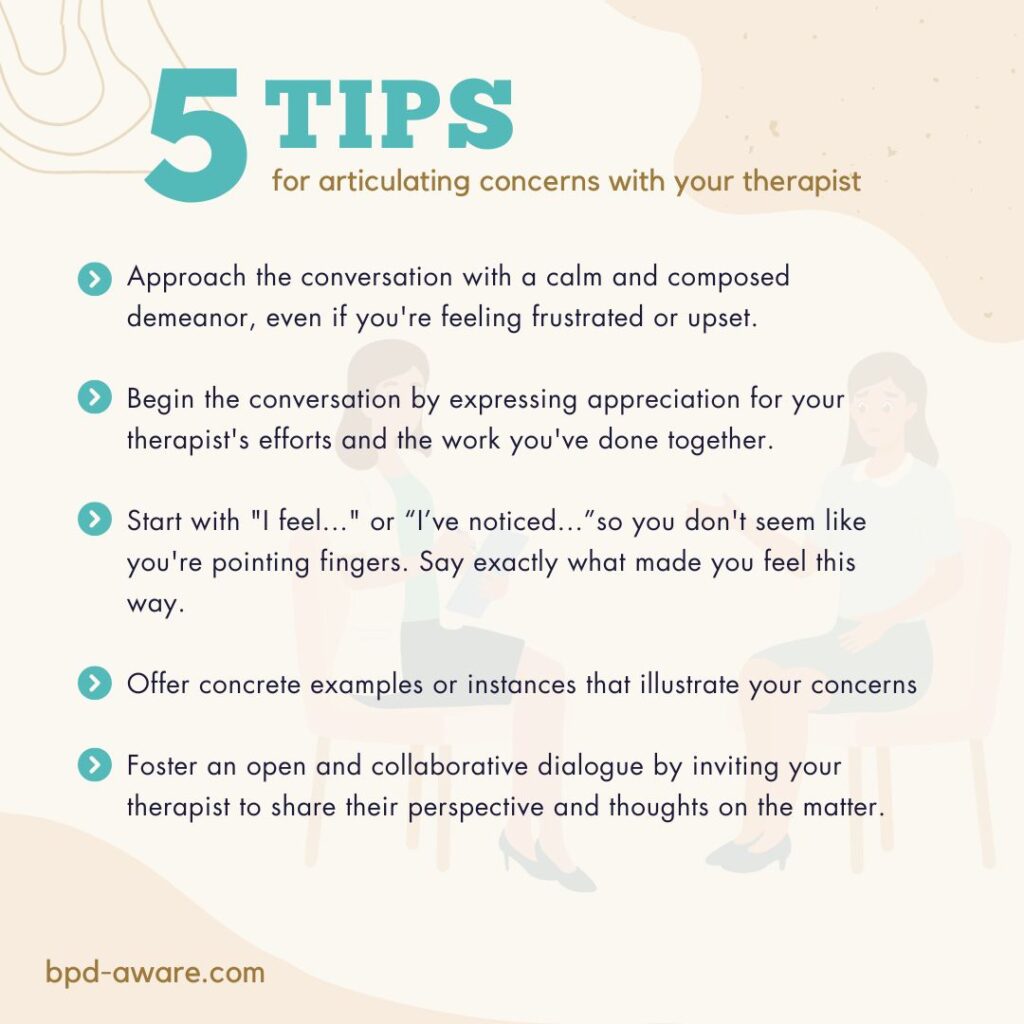
Articulate concerns respectfully: Talk to your therapist in a respectful and non-confrontational manner. Share the exact issues or disagreements you have with their approach or advice. Use “I” statements to share how you feel and what you’ve been through without blaming them directly.
Ask questions for clarification: Get more info from your therapist to fully understand their side. Ask open questions to dive deeper into their thinking on certain advice or steps. This makes talking better and helps both of you understand each other.
Speak up for what you need and want: Highlight how important it is for therapy to match your personal needs and goals. Share openly what you aim to get from therapy and how certain parts of therapy might be slowing you down. Stand up for changes that better meet your wishes and goals.
Think about getting another opinion: If you still feel unsure or unresolved after talking with your therapist, think about getting advice from another mental health professional. Talking to someone else can give new views and thoughts on the situation. Plus, it can confirm your feelings and help you make smart choices about your therapy journey.
Look into other therapy ways or methods: Be ready to look into different therapy methods that might fit you better. While Dialectical Behavior Therapy (DBT) is the most common form of therapy used to treat BPD, it’s not for everybody. Mentalization-Based Therapy (MBT) or Schema Therapy (amongst others) may be better suited for you. Look up various therapy actions and ways that meet your needs and likes. Talk about these options with your therapist and think about using them in your treatment plan.
Think about if it’s a bad match: In the end, think about if the issue is because you and your therapist don’t match. Think about if you have big differences in how you talk, what you value, or what you prefer in therapy that might be making therapy less effective. If needed, think about finding a new therapist who matches your needs and goals better.
Dealing with disagreements with your therapist needs patience, clear conversation, and being open to other ways of doing things. By taking steps early to talk about what bothers you and standing up for what you need, you can build a better bond with your therapist. If you feel like the patient-therapist relationship can’t be salvaged, it’s likely time to seek another option.
Final Thoughts
Navigating the complexities of BPD while addressing disagreements with your therapist demands bravery, self-insight, and dedication to your healing. Identifying moments when you feel your therapist might not be getting it right is a key action in advocating for yourself, ensuring your therapy remains beneficial and tailored to your requirements.
It’s important to understand that therapy is a joint venture, and your input is of significant importance. Trusting your gut and speaking up when something seems off plays a crucial part in taking care of yourself and feeling empowered. This could mean respectfully sharing your concerns, standing up for your own needs and aspirations, or even contemplating a switch to a therapist who is a better match for your beliefs, all in the name of prioritizing your mental health.
The ultimate aim of therapy is to aid you in dealing with BPD’s hurdles while encouraging personal growth and healing. By actively participating in your therapy, and procuring the necessary support and resources, you can foster a more rewarding and effective therapeutic experience.
You are worthy of empathetic and efficient care, and it’s perfectly acceptable to make moves that ensure your therapy supports your mental health and well-being.
Sources, Resources, and Further Reading
- I Don’t Like My Therapist (Is It Them or Is It Me?): https://blog.opencounseling.com/what-if-i-dont-like-my-therapist/
- What to Consider if You Want to Switch Therapists: https://www.talkspace.com/blog/switch-therapists-how-to/
- How to Change Therapists: 5 Steps: https://psychcentral.com/health/changing-therapists
- What If You and Your Therapist Disagree?: https://www.sondermind.com/resources/articles-and-content/what-if-you-and-your-therapist-disagree/